Department of Health and Human Services
DEPARTMENTAL APPEALS BOARD
Appellate Division
Borgess Medical Center
Docket No. A-19-19, A-19-20
Decision No. 3106
FINAL DECISION ON REVIEW OF ADMINISTRATIVE LAW JUDGE DECISION
These related appeals arise from a June 5, 2015 reconsidered determination by the Centers for Medicare & Medicaid Services (CMS) that three physicians' clinics purportedly owned and operated by Borgess Medical Center (Borgess),1 an acute care hospital, did not meet the public awareness requirement in 42 C.F.R. § 413.65(d)(4). The basis for that reconsidered determination was that exterior signs at the three clinics and Borgess's website did not clearly identify the clinics as outpatient departments of Borgess. The public awareness requirement, among others, had to be met in order for Borgess, a Medicare-participating provider, to treat the clinics as "provider-based" (that is, as parts of the hospital) for Medicare payment purposes.
On September 11, 2018, an administrative law judge (ALJ) sustained the reconsidered determination, holding that the clinics did not meet the public awareness requirement "prior to October 2, 2015." Borgess Med. Ctr., DAB CR5185 (ALJ Decision). The ALJ further concluded that the clinics "met all requirements for provider-based status," including the public awareness requirement, "as of October 2, 2015," and that such status became "effective" on that date pursuant to 42 C.F.R. § 413.65(o). Id. at 1, 16.
Both parties have appealed the ALJ's decision. Borgess challenges only the part of the ALJ Decision unfavorable to it – namely, the ALJ's conclusion that the clinics did not meet the public awareness requirement before October 2, 2015. CMS challenges the ALJ's conclusion that the clinics met all requirements for provider-based status as of October 2, 2015 and that such status became effective on that date. CMS thus wants the Board to uphold only the ALJ's conclusion that the clinics did not meet the public awareness requirement before October 2, 2015.
Page 2
As we explain below, the issue before the ALJ was whether the three clinics met the public awareness requirement in 42 C.F.R. § 413.65(d)(4). The issues of when the clinics met the public awareness requirement and when they met all other requirements for establishing provider-based status were not before the ALJ. Accordingly, we conclude that the ALJ erred in reaching and deciding the "effective date" of the clinics' meeting the public awareness requirement and all other provider-based status requirements. We affirm only the ALJ's conclusion that the three clinics did not meet the public awareness requirement in 42 C.F.R. § 413.65(d)(4) before October 2, 2015; we vacate the ALJ's conclusion that the three clinics met all provider-based status requirements as of October 2, 2015. Our vacating the ALJ Decision in part effectively results only in a conclusion that the clinics did not meet the public awareness requirement in 42 C.F.R. § 413.65(d)(4).
Legal Background
A. Provider-based entities and billing
The Medicare program pays participating hospitals and other healthcare "providers" for health care services they furnish to program beneficiaries. Social Security Act (Act) §§ 1811, 1812(a) (providing that Medicare program benefits include payment for inpatient hospital services); 42 C.F.R. Part 419 (establishing prospective payment systems for hospital outpatient department services); 42 C.F.R. § 400.202 (defining the term "provider," for Medicare program purposes, to include hospitals).
For Medicare payment purposes, CMS recognizes that a hospital may own and operate other types of healthcare facilities or organizations, such as physicians' offices, that are located on or off the hospital's campus. See Final Rule, 65 Fed. Reg. 18,434, 18,504 (April 7, 2000). Subject to various statutory and regulatory limitations and conditions, CMS permits a hospital to treat such subordinate entities as "provider-based," and to bill their services to Medicare as outpatient hospital services. See id.; Shady Grove Adventist Hosp., DAB No. 2221, at 3 (2008) (citing Proposed Rule, 63 Fed. Reg. 47,552, 47,587-88 (Sept. 8, 1998)), aff'd sub nom. Adventist Healthcare, Inc. v. Sebelius, AW-09-00559, 2010 WL 3038917 (D. Md. July 30, 2010).2
Page 3
For some services, provider-based billing may result in Medicare payment exceeding what the program would pay for the same services if they were furnished in a "free-standing" facility or organization (that is, an entity not integrated with, or part of, a provider).3 Shady Grove at 3. Provider-based billing "may also serve to increase the coinsurance liability of Medicare beneficiaries who receive covered services in [the provider-based] facility." Id.
Prior to 2000, the Medicare program's criteria for designating a facility or organization as provider-based were found largely in Program Memorandum (PM) A-96-7, issued by the Health Care Financing Administration (HCFA), CMS's predecessor. 65 Fed. Reg. at 18,504; Shady Grove at 15.
B. Regulatory requirements for provider-based status (42 C.F.R. § 413.65)
In 2000, CMS promulgated 42 C.F.R. § 413.65, which superseded PM A-96-7 and established requirements for a facility or organization to qualify for "provider-based status." 65 Fed. Reg. at 18,504.
The Act does not define the term "provider-based." However, section 413.65 defines "provider-based status" to mean the "relationship between a main provider and a provider-based entity or a department of a provider, remote location of a hospital, or satellite facility, that complies with the provisions of this section." 42 C.F.R. § 413.65(a)(2) (italics added). The term "main provider" is defined as "a provider [such as a hospital] that either creates, or acquires ownership of, another entity to deliver additional health care services under its name, ownership, and financial and administrative control." Id. The term "department of a provider" (which covers the physician clinics at issue in this case) is defined in part as "a facility or organization that is either created by, or acquired by, a main provider for the purpose of furnishing health care services of the same type as those furnished by the main provider under the name, ownership, and financial and administrative control of the main provider, in accordance with the provisions of this section [413.65]." Id. The regulation defines the term "provider-based entity," in part (and similar to the term "department of a provider"), as "a provider of health care services . . . that is either created by, or acquired by, a main provider for the purpose of furnishing health care services of a different type from those of the main provider under the ownership and administrative and financial control of the main provider . . . ." Id. A provider and its subordinate facility (i.e., its "department of a provider" or "provider-based entity") could achieve cost savings by "shar[ing] overhead costs and . . . revenue-producing assets." Shady Grove at 3.
Page 4
Section 413.65 distinguishes a facility or organization qualifying for provider-based status from a "[f]ree-standing facility." 42 C.F.R. § 413.65(a)(2). The latter is "an entity that furnishes health care services to Medicare beneficiaries and that is not integrated with any other entity as a main provider, a department of a provider, remote location of a hospital, satellite facility, or a provider-based entity." Id.
C. The "public awareness" requirement of section 413.65
Under 42 C.F.R. § 413.65, a facility or organization seeking provider-based status must meet all applicable requirements in that section concerning licensure, integration of clinical services, integration of financial operations, and "public awareness." 42 C.F.R. § 413.65(d).4 The "public awareness" requirement at issue in this case is found in section 413.65(d)(4), which states:
Public awareness. The facility or organization seeking status as a department of a provider, a remote location of a hospital, or a satellite facility is held out to the public and other payers as part of the main provider. When patients enter the provider-based facility or organization, they are aware that they are entering the main provider and are billed accordingly.[5]
In the preamble to its 2000 rulemaking, CMS emphasized that an "objective in issuing specific criteria for provider-based status [was] to ensure that higher levels of Medicare payment and increases in beneficiary liability for deductibles or coinsurance (which can all be associated with provider-based status) are limited to situations where the facility or organization is clearly and unequivocally an integral and subordinate part of a provider." 65 Fed. Reg. at 18,506. CMS also commented that the public awareness requirement was "needed to help ensure that beneficiaries are protected from unexpected deductible and coinsurance liability." Id. at 18,522.
D. The 2002 amendments to section 413.65
As originally promulgated, section 413.65(b) prohibited a main provider from billing Medicare for a facility's services as provider-based unless the provider first applied for
Page 5
and obtained a determination by CMS that the facility was provider-based. 65 Fed. Reg. at 18,538. In order "[t]o provide an administrative appeals process" to contest a denial by CMS of an application for provider-based status, the 2000 rulemaking revised the list of appealable "initial determinations" in 42 C.F.R. § 498.3 to include, as specified in paragraph (b)(2), "determinations with respect to . . . [w]hether a prospective department of a provider, remote location of a hospital, satellite facility, or provider-based entity qualifies for provider-based status under § 413.65 of this chapter." Id. at 18,505, 18,524, 18,549. The 2000 rulemaking also revised section 498.3(b)(2) to include a "determination" by CMS about "whether . . . a facility or entity currently treated" as provider-based "no longer qualifies for that status under § 413.65 of this chapter." Id. at 18,524, 18,549.
In 2002, CMS amended section 413.65 by removing the requirement (in paragraph (b)) that a provider apply for and obtain a determination by CMS of a facility's or organization's provider-based status before billing its services as provider-based. The 2002 amendments substituted a voluntary process under which a provider may obtain a determination of provider-based status by submitting to CMS an "attestation" that the affiliated facility or organization meets all applicable requirements for that status. CMS then may use that submission to "make a determination as to whether the facility or organization is provider-based." 42 C.F.R. § 413.65(b)(3); see also 67 Fed. Reg. 49,982, 50,084-85, 50,087, 50,114-15 (Aug. 1, 2002). Thus section 413.65, as amended in 2002, does not require the main provider to obtain a determination of a subordinate facility's provider-based status before billing that facility's services as provider-based, but the provider's belief that the facility is provider-based does not legally entitle the provider to treat it as such for Medicare billing and payment purposes. 42 C.F.R. § 413.65(b)(1) (providing that "[a] facility or organization is not entitled to be treated as provider-based simply because it or the main provider believe[s] it is provider-based").
Section 413.65(j) – titled "Inappropriate treatment of a facility or organization as provider-based" – specifies how CMS is to handle such inappropriate treatment. Section 413.65(j) provides that if CMS (1) learns that a provider has treated as provider-based a facility or organization for which the provider did not request a determination of provider-based status using the voluntary attestation process, and (2) "determines that the facility or organization did not meet the requirements for provider-based status," then "CMS will":
- notify the provider "that payments for past cost reporting periods may be reviewed and recovered" and "that future payments for services in or of the facility or organization will be adjusted";
- "adjust the amount of future [Medicare] payments to the provider for services of the facility or organization" (that had been inappropriately treated as provider-based) based on an estimate of the "amounts that would be paid for
Page 6
the same services furnished by a freestanding [non-provider-based] facility";
- "recover [subject to certain limitations] the difference between the amount of payments that actually was made" for services at the facility or organization inappropriately treated as provider-based, and "the amount of payments that CMS estimates should have been made, in the absence of compliance with the provider-based requirements, to that provider for services at the facility or organization for all cost reporting periods subject to reopening . . ."; and
- "continue payments to the provider for services of the facility or organization" inappropriately treated as provider-based "only in accordance with" paragraph (j)(5).
42 C.F.R. § 413.65(j)(1)(i)-(ii), (j)(3), (j)(4), (j)(5). These provisions superseded the provisions of section 413.65(j), as promulgated in 2000, which specified certain consequences if a provider improperly treated a facility as provider-based without first having obtained CMS's approval of that status. 65 Fed. Reg. at 18,540-41.
Section 413.65(j)(5), titled "Continuation of payment," clarifies the circumstances under which Medicare payment for a facility's or organization's services will or will not continue after issuance of a "notice of denial of provider-based status" (that is, a notice to the provider that it has inappropriately treated the facility or organization as provider-based). The notice of denial of provider-based status will ask the provider to notify CMS within 30 days if the provider intends to seek a CMS determination of provider-based status or if the facility or organization intends to enroll in Medicare as a freestanding facility. 42 C.F.R. § 413.65(j)(5)(i). If the provider so notifies CMS, then Medicare payments for the facility's or organization's services will continue (in "adjusted" amounts applicable to a freestanding facility, as specified in section 413.65(j)(4)) for not longer than six months, under several additional conditions. Id. § 413.65(j)(5)(iii). Those conditions for continuing payment are met if "the provider or the facility or organization or its practitioners":
(A) Submits, as applicable, a complete request for a determination of provider-based status or a complete enrollment application and provide[s] all other required information within 90 days after the date of notice [of CMS's denial of provider-based status]; and
(B) Furnishes all other information needed by CMS to make a determination regarding provider-based status or process the enrollment application, as applicable, and verifies that other billing requirements are met.
Id. "If the necessary applications or information are not provided, CMS will terminate all
Page 7
payment to the provider, facility, or organization as of the date CMS issues notice that necessary applications or information have not been submitted." Id. § 413.65(j)(5)(v).
In short, under the process established by section 413.65(j), if CMS determines that a provider has inappropriately treated a subordinate facility or organization as provider-based, then CMS will not regard the facility or organization as provider-based for Medicare payment purposes unless or until the provider files an application or attestation requesting that CMS determine the facility's or organization's entitlement to provider-based status.
The effective date of any determination by CMS to approve a request for provider-based status is governed by section 413.65(o). Paragraph (2) of that section states that "if a facility or organization is found by CMS to have been inappropriately treated as provider-based under paragraph (j) of this section," then "CMS will not treat the facility or organization as provider-based for payment purposes until CMS has determined, based on documentation submitted by the provider, that the facility or organization meets all requirements for provider-based status." 42 C.F.R. § 413.65(o)(2). Paragraph (2) of section 413.65(o) is an application of the general rule in paragraph (1), which states that "[p]rovider-based status for a facility or organization is effective on the earliest date all of the requirements [for such status] have been met." Id. § 413.65(o)(1).
E. CMS's 2003 issuance of sub-regulatory guidance
In 2003, CMS issued PM A-03-030, which states that it superseded program instructions in two other CMS program manuals and "provides information on the background of the provider-based regulations [as revised in 2002] and notifies [Medicare program contractors] of the actions [they] are to take to implement the revised regulations." CMS Ex. 19, at 1. PM A-03-030 contains the following passage regarding the public awareness requirement:
As documentation [of compliance with section 413.65(d)(4)], the provider may maintain examples that show that the facility is clearly identified as part of the main provider (i.e., a shared name, patient registration forms, letterhead, advertisements, signage, Web site). Advertisements that only show the facility to be part of or affiliated with the main provider's network or healthcare system are not sufficient.
Id. at 6 (italics omitted).
Page 8
Case Background
Borgess is a Medicare-participating acute-care hospital located in Kalamazoo, Michigan. Joint Stipulations of Fact (Jt. Stip.) ¶¶ 1-3; Borgess Request for Review (B. RR) at 1. At all times relevant to the parties' dispute, Borgess was part of a healthcare network known as "Borgess Health" (or "Borgess Health Alliance"). Jt. Stip. ¶ 3; Borgess Exhibit (B. Ex.) 18; B. Ex. 24, ¶ 4. Borgess Health also included an entity named ProMed Healthcare. B. Ex. 24, ¶ 5; CMS Ex. 18, at 30; B. Ex. 18, at 1-2 (screenshot of Borgess Health website listing various "Borgess Corporate Entities," including ProMed Healthcare, Inc.).
In 2009 and 2010, Borgess began to treat certain off-campus physician clinics named "ProMed Physicians Family Practice" as provider-based for Medicare billing purposes. See Jt. Stip. ¶¶ 6-7. The clinics in question were located in Mattawan, Richland, Three Rivers, and Portage, Michigan. Id. ¶ 6. Borgess treated the clinics as provider-based without first having sought a determination from CMS that they qualified as such. Id. ¶ 7; B. Ex. 10, ¶ 15.
In 2014, CMS undertook to determine whether the ProMed Physicians clinics in Mattawan, Richland, Three Rivers, and Portage met the public awareness requirement and other requirements for provider-based status. CMS's investigation was prompted by a Medicare beneficiary's complaint that he had unexpectedly received a hospital bill after visiting a physician at one of the clinics. See CMS Ex. 1, at 4; CMS Ex. 2, at 2-3.
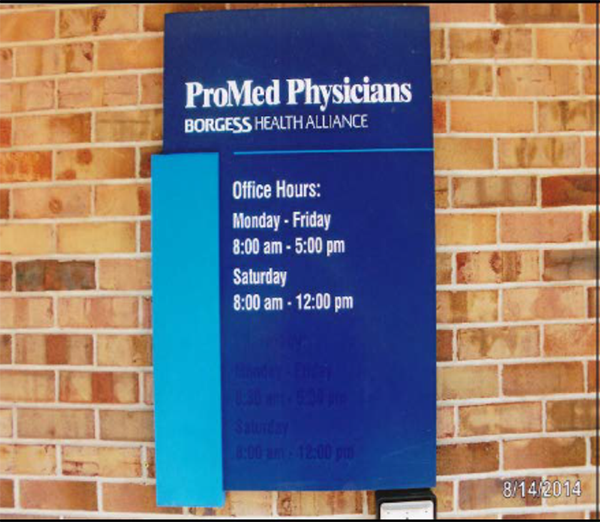
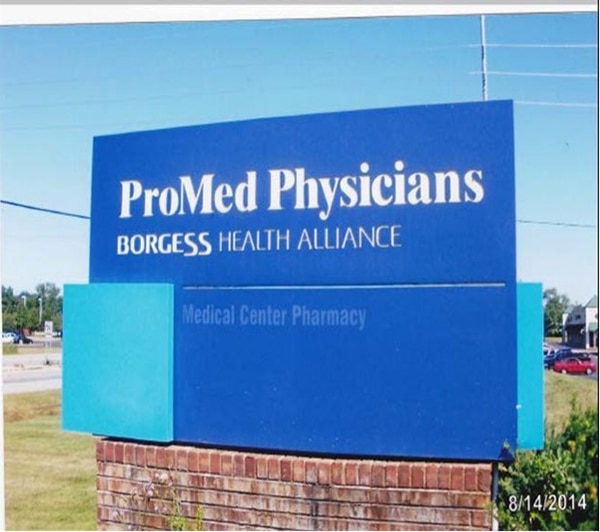
In assessing whether the clinics were compliant with the public awareness requirement, CMS examined, among other material, the clinics' exterior signs and Borgess Health's website. See CMS Exs. 3-6 (Aug. 2014 photographs); CMS Ex. 7 (September 4, 2014 Borgess Health webpage containing information about "ProMed Physicians – Family Practice," describing the practice as an "affiliate of Borgess Health," and listing the Mattawan, Portage, Richland, and Three Rivers clinics and their addresses). In August 2014, the clinics' exterior signs appeared as follows:
Page 9
Mattawan Clinic (CMS Ex. 3)

Page 10
Mattawan Clinic (CMS Ex. 3)

Page 11
Richland Clinic (CMS Ex. 4)

Page 12
Three Rivers Clinic (CMS Ex. 5)

***The top two lines of the sign near the door read:
ProMed Physicians
BORGESS HEALTH ALLIANCE
Page 13
Three Rivers Clinic (CMS Ex. 5)
Page 14
Three Rivers Clinic (CMS Ex. 5)
Page 15
Portage Clinic (CMS Ex. 6)

Page 16
Portage Cinic (CMS Ex. 6)

Page 17
Portage Clinic (CMS Ex. 6)

Page 18
As these photographs (taken in August 2014) reflect, signs outside the Mattawan, Richland, and Three Rivers clinics identified them as part of "Borgess Health," "Borgess," or "Borgess Health Alliance." CMS Ex. 3-5. Two of the three signs outside the Portage clinic, and building lettering, identified that clinic as part of "Borgess Woodbridge Hills," a campus of offices or facilities providing pharmacy, outpatient surgery, and other medical or healthcare services. CMS Ex. 6, at 1, 3. One photograph of the signage outside the Portage clinic does not show "Borgess," "Borgess Health," or "Borgess Health Alliance." Id. at 2.
A. CMS's initial determination under 42 C.F.R. § 413.65(j)(1)
On September 19, 2014, CMS issued an initial determination notifying Borgess that it had not met two requirements for treating the ProMed Physicians clinics in Mattawan, Richland, Three Rivers, and Portage, Michigan as provider-based. CMS Ex. 2. The two requirements were: the public awareness requirement in 42 C.F.R. § 413.65(d)(4); and the notice-of-coinsurance-liability requirement in 42 C.F.R. § 413.65(g)(7). Id. (The latter requirement is not at issue in this case.)
In support of its finding that Borgess had not met the public awareness requirement, CMS stated, in relevant part:
The ProMed Physicians Family Practice locations are not sufficiently held out to the public as departments of Borgess Medical Center in Kalamazoo, Michigan (i.e., the hospital that claims these clinics as having provider-based status to it). The public awareness criterion for having provider-based status requires that patients who enter a provider-based department are aware that they are entering the main provider. Rather than being held out as departments of Borgess Medical Center, they are held out as "ProMed Physicians" and "Borgess Health." The signage for these facilities in no way indicates that they are part of Borgess Medical Center, the specific hospital located in Kalamazoo, Michigan.
The Borgess Health System is comprised of three separately-certified Medicare hospitals and a large number of other healthcare facilities. In order to satisfy the public awareness criterion, a provider-based department, remote location, or satellite facility must be held out to the public as part of the specific hospital that is the main provider. Signage indicating that the physician office is "ProMed Physicians" and "Borgess Health" only implies that the [ProMed Physicians] offices are associated with the Borgess Health system. Proper signage is vitally important to identify a healthcare facility as a provider-based hospital department and to satisfy the public awareness criterion. The "ProMed Physicians" and "Borgess Health" signage does not meet the requirement . . . .
Page 19
The Borgess website . . . does not help to clarify that the "ProMed Physicians" locations are departments of a hospital. The website merely identifies the ProMed clinics as "affiliates" of Borgess Health [referring to the website screenshot in CMS Ex. 2, at 6], again only implying that the practices are associated with the health system and not an integrated part of one of the three Borgess hospitals. The description of the family practice clinics in no way indicates that the facilities are anything other than freestanding physician offices.
The public awareness requirement . . . is important and applies to all provider-based departments, remote locations, and satellite facilities. Medicare patients generally face higher cost-sharing obligations at provider-based departments when compared with a freestanding facility offering the same healthcare services. The main provider's requirement to represent these facilities as a part of the main provider informs patients that they are entering a hospital and permits them to make informed decisions about their health care prior to receiving services.
CMS Ex. 2, at 2 (italics added).
Based on the noncompliance findings, the initial determination notified Borgess of the remedies CMS was imposing and Borgess's responsive options. CMS would, in accordance with 42 C.F.R. § 413.65(j)(1)(ii), "recover overpayments made from [September 19, 2014] back to the date on which [Borgess] began inappropriately treating the [four ProMed clinics] as provider-based." Id. at 3. Borgess had three options for clarifying or resolving the clinics' status with the Medicare program:
- Option 1 – "notify CMS in writing within 30 days . . . that [it] intends to make the changes needed for the [clinics] to comply with the provider-based rules" and that it "intends to seek a determination of provider-based status for [the clinics]";
- Option 2 – "notify CMS in writing within 30 days . . . that the [clinics] (or . . . the practitioners who staff [them]) will be seeking to enroll and meet other requirements to bill for services in a freestanding facility"; and
- Option 3 – "choose not to notify CMS" with respect to the other two options, in which case "all payment [would] end as of the 30th day after the date of the notice."6
Page 20
Id. at 3-4. If Borgess elected Option 1, Medicare would continue to pay for the clinics' services at rates applicable to freestanding facilities (but for no longer than six months), provided that Borgess submitted a "complete request (not an attestation) for a provider-based determination and all other required information within 90 days," and that "[i]f the necessary application or information [was] not provided, CMS [would] terminate all payment . . . as of the date CMS issue[d] notice that necessary applications or information ha[d] not been submitted." Id. at 3. Regardless of which option Borgess chose, it could appeal the "denial of provider-based status" in accordance with the procedures in 42 C.F.R. Part 498. Id. at 4.
By letter dated November 5, 2014, Borgess informed CMS that it had elected Option 1. CMS Ex. 31, at 1. Borgess stated that it would "work with [CMS] to obtain approval of signage and branding that will satisfy the provider-based requirements and then submit a determination request for approval of provider-based status for" the four ProMed Physicians clinics. Id. Borgess also notified CMS that it would "separately file a Request for Reconsideration . . . seeking a redetermination of the revocation of provider-based status for the [clinics]." Id. at 2.
B. Borgess's reconsideration request and post-request correspondence, and CMS's reconsidered determination
On December 4, 2014, Borgess filed a request for reconsideration, asserting that it had not violated either the public awareness or the notice-of-coinsurance-liability requirement, and that the four clinics in question were "clearly integrated with the Hospital [Borgess Medical Center] and held out to the public as part of the hospital." CMS Ex. 32, at 1-2.
With respect to the public awareness requirement, Borgess contended that the clinics' exterior signs adequately communicated that the clinics were part of the hospital. Borgess emphasized that all of the signs contained the name "Borgess"; that "the public generally associates [that name] with the Hospital"; that the "addition of the words Health or Health Alliance to the word Borgess does not negate the impact of the use of the Borgess logo and identification of that as a hospital within the Kalamazoo [Michigan] market." Id. at 3-5. Borgess also emphasized that the Portage clinic's exterior signs used only the name "Borgess" and thus any concern CMS harbored about the names "Borgess Health" and "Borgess Health Alliance" was irrelevant in judging whether that particular clinic met the public awareness requirement. Id. at 5.
Borgess further contended that the absence of the words "Medical Center" adjacent to the "Borgess" name on the clinics' exterior signs was not "solely determinative," and that the clinics' compliance could be demonstrated by showing that they provided patients (either in-person or online) with other material identifying them as parts of the hospital. Id. at 3, 5. In support of these contentions, Borgess relied upon Johns Hopkins Health Systems,
Page 21
DAB CR598 (1999), aff'd, DAB No. 1712 (1999), which held that an oncology center that Johns Hopkins Hospital treated as provider-based had met the then-existing public awareness standard in PM A-96-7. Id. at 2-3. Borgess asserted that Johns Hopkins "demonstrates that a hospital does not necessarily need to use its entire name in order to meet the public awareness requirement" and "clearly indicate[s] that when evaluating the public awareness standard CMS must look to the record as a whole and should not pick and choose specific pieces of evidence." Id. at 3, 5.
As evidence that the clinics used means other than exterior signs to meet the public awareness requirement, Borgess submitted copies of three documents or notices allegedly provided, or made available, to patients inside the clinics. Id. at 5, 69-73. One document, titled "Important Notice," states: "As you may know, Borgess Medical Center owns and operates this physician office. To comply with Medicare regulations, we create two separate bills for your office visit. Specifically, we generate a bill for the physician and another bill for the facility. You will receive a separate Medicare explanation of benefits . . . for each." Id. at 73 (emphasis in original). The "Important Notice" further states that a patient's coinsurance responsibility might "change" (that is, increase) because of "this Medicare billing requirement" and gives examples of physician and "facility" charges (and associated coinsurance amounts) for a "common physician visit" in the clinic. Id. A second document, titled "Provider-Based Medicare Billing," poses the question, "What does Provider-Based Medicare billing mean?" and gives the following answer: "This is a Medicare status for hospital clinics that comply with specific Medicare regulations. As a result of this status, Borgess Medical Center will bill Medicare in two parts. You will receive bills from Borgess Medical Center [for a "facility fee"] and your physician office" (for the professional services of the physician or other practitioner). Id. at 71-72. The Provider-Based Medicare Billing notice also contains estimates of patient coinsurance amounts and includes the hospital's name and address at the bottom. Id. at 72. The third document is a form titled "General Consent for Treatment – Physician Office Practices and Off-Campus Departments." Id. at 69. The "Borgess" wordmark appears at the top of the consent form, and the form uses the name "Borgess" throughout. Id. at 69-70. In addition to these patient forms, Borgess provided with its reconsideration request screenshots of webpages from the Borgess website that listed numerous "Borgess Locations" – including "ProMed Physicians Family Practice" clinics in Mattawan, Richland, Three Rivers, and Portage – just below the Borgess wordmark and a photograph of the Borgess campus.7 Id. at 4, 64-68.
Page 22
On April 28, 2015, following up on a telephone conference between the parties, Borgess wrote to CMS about its plans to change the signs outside the ProMed Physicians clinics. CMS Ex. 34. Borgess attached to its April 28th correspondence a mockup of the modified signs and asked CMS for "input before any of the signs are installed." Id. at 1. Borgess also informed CMS that it had updated its website "to more clearly indicate that the clinics are operated as a part [of] the Hospital." Id.
On June 5, 2015, CMS issued a "partially unfavorable" reconsidered determination. CMS Ex. 1, at 1. CMS determined that the ProMed Physicians clinics in Mattawan, Richland, Three Rivers, and Portage met the notice-of-coinsurance-liability requirement. Id. at 3. CMS also determined that the Portage clinic met the public awareness requirement, stating: "Accepting [Borgess's] argument that local residents closely associate the stand-alone name ‘Borgess' with the hospital, we are persuaded that the primary and prominent use of the logo ‘Borgess' at the facility at 7901 Angling Road [see CMS Ex. 6] is – when considered with other evidence tying the facility to the main provider – sufficient to allow a finding that this particular facility is held out to the public as part of Borgess Medical Center." Id. However, for the following reasons, CMS upheld its initial determination that the Mattawan, Richland, and Three Rivers clinics did not satisfy the public awareness requirement:
Unlike the Portage facility, the signage for [the Matawan, Richland and Three Rivers clinics] identifies them first and foremost as "ProMed Physicians" clinics and not as integral and subordinate parts of Borgess Medical Center. . . . [Before the Hospital began operating the ProMed clinics in Mattawan, Richland, and Three Rivers as provider-based], ProMed Physicians had a history of operating many freestanding physician clinics known to the people of the Kalamazoo area. The ProMed Physician clinics at issue here were treated as provider-based to Borgess Medical Center without sufficient re-branding to clearly identify that these clinics now operate and charge as hospital outpatient departments. It is possible that patients, who had seen their ProMed physicians in those freestanding physician offices, continued to see the same physicians, sometimes in the same offices, only now in a hospital outpatient setting. When well-known freestanding physician offices transition to provider-based hospital departments, CMS expects the main provider to ensure that this transition is clearly communicated to the public, including through signage identifying the facilities as now being an integrated part of a hospital, in this case Borgess Medical Center.
While the signage for [the Mattawan, Three Rivers, and Richland] facilities includes reference to "Borgess Health" or "Borgess Health Alliance," this is insufficient to clearly identify them as provider-based departments of their main provider, the hospital named Borgess Medical Center. While we have
Page 23
accepted [the] argument that Borgess Medical Center is known locally simply as "Borgess," it does not follow that use of any phrase that includes the word "Borgess" shows that a facility is sufficiently associated with Borgess Medical Center to satisfy the public awareness requirement.
In fact, Borgess Health is a sizable health system in southwest Michigan and is comprised of three separately-certified hospitals (Borgess Hospital, Borgess Lee Memorial Hospital, and Borgess Medical Center) and a number of other locations. Many health systems operate freestanding physician clinics. The term "Borgess Health Alliance," similarly refers to much more than the Borgess Medical Center alone. A provider-based location must hold itself out to the public as part of the main provider, not as part of a group that also includes the main provider. CMS has long-standing guidance, CMS Program Memorandum A-03-030, explaining that "only show[ing] the facility to be part of or affiliated with the main provider's network or healthcare system" is not enough to show the facility is "clearly identified as part of the main provider." Merely identifying the ProMed Physicians Family Practice facilities as part of the health system, or in alliance with the health system, does not identify them to the public as part of Borgess Medical Center specifically. In fact, a Medicare beneficiary visiting the Three Rivers Facility submitted a complaint and stated that he did not know he was receiving care in a hospital facility, which supports the conclusion that the signage, which is similar in all three ProMed Physicians Family Practice locations, is insufficient to alert a beneficiary that he or she is entering the main provider.
The Borgess Health website . . . did not clarify the relationship between the ProMed Physicians Family Practice and the hospital called Borgess Medical Center. The website information, which has since been updated, identified the facilities only as ProMed Physicians locations, with an indeterminate "affiliation" with the larger Borgess Health system, not specifically as part of Borgess Medical Center, the main provider.
Id. at 3-5. The reconsidered determination noted that Borgess had submitted information about changes it "plan[ned] to make to come into compliance with regulatory requirements" but that this information was "not relevant to the reconsideration" because it "cannot show the [clinics] met regulatory requirements at the applicable time" (that is, as of the date of the adverse determinations). Id. at 3. The reconsidered determination also advised Borgess that "further action w[ould] be taken" pursuant to 42 C.F.R. § 413.65(j)(1)(ii) to recover Medicare overpayments resulting from the inappropriate treatment of the Mattawan, Richland, and Three Rivers clinics as provider-based. Id. at 5. Finally, the reconsidered determination notified Borgess that it could, if dissatisfied with the result, request a hearing before an administrative law judge. Id.
Page 24
C. CMS's June 8, 2015 correspondence, Borgess's hearing request, and the proceedings before the ALJ
On June 8, 2015 (three days after it issued the reconsidered determination), CMS sent Borgess a letter responding to the latter's April 28th correspondence. B. Ex. 19. Cautioning that its letter was "intended as informal guidance only and . . . may not be relied upon to show compliance with any aspect of the provider-based status regulations," CMS stated that Borgess's modified signs for the Mattawan, Richland, and Three Rivers clinics "appear similar to the current signage at the Portage facility, a location that CMS has accepted as provider-based," and that "proposed changes to the branding and website content that have been completed for the ProMed Physicians sites appear to reflect that the ProMed Physicians Family Practice sites are operated as part of Borgess Medical Center." Id. at 2. Before providing its "informal guidance," CMS reminded Borgess, "in accordance with 42 C.F.R. § 413.65(o)(2)," that if it wished to treat the Mattawan, Richland, and Three Rivers clinics as provider-based, then it needed to "submit complete attestations of provider-based status for each facility," and CMS needed to determine, based on those submissions "and any associated material," that the facilities complied with "all of the provider-based requirements and obligations . . . ." Id. at 1.
On July 31, 2015, Borgess requested an ALJ hearing to challenge the "denial of provider-based status with respect for the" Mattawan, Richland, and Three Rivers clinics. Jt. Stip. ¶ 14. Between November 2015 and March 2016, the parties exchanged documentary evidence and written legal argument. Among the exhibits proffered by Borgess were declarations by Richard Felbinger, Senior Vice President and Chief Financial Officer of Borgess Health, who averred that Borgess Medical Center was founded in 1889 and has been located on the same campus since 1917; that "[d]ue to its long history and prominent role in the region, Borgess Medical Center is inextricably associated with the name ‘Borgess' throughout southwest Michigan"; and that Borgess Medical Center "is the flagship hospital of the Borgess Health system." B. Ex. 10, ¶ 5. Referring to the previously mentioned documentation submitted with Borgess's reconsideration request, Felbinger further averred that "every patient who sets foot" in the Mattawan, Richland, and Three Rivers clinics is presented with "multiple signs, forms, and documents" identifying the clinics as part of Borgess Medical Center. Id. ¶ 8. In particular, said Felbinger, "[a] version" of the "Important Notice" concerning Medicare billing for office visits (and stating that "Borgess Medical Center owns and operates this physician office") has been displayed on a sign "[a]t the reception desk" of the Mattawan, Richland, and Three Rivers clinics "since each began billing as provider-based," and that each clinic also makes available, as a "brochure," the "Provider-Based Medicare Billing" notice. Id. ¶¶ 9-11 (referring to CMS Ex. 32, at 71-73, and citing B. Exs. 3-5 (photographs of interior signs)). In addition, said Felbinger, "[b]efore receiving care" at any of the clinics, "patients are asked to read and sign [the] treatment consent form, both pages of which bear the Borgess wordmark," as well as a Notice of Privacy Practices containing that wordmark. Id. ¶¶ 12-13 (citing CMS Ex. 32, at 69-70 and B. Ex. 6).
Page 25
Before filing their opening briefs, the parties filed a Joint Stipulation of Facts, a Joint Statement of Issues Presented, and a Joint Settlement Status Report. In the Joint Settlement Status Report, the parties "waive[d] oral hearing and request[ed] a decision on the briefs and written record, including the evidence submitted as part of their respective pre-hearing exchanges." Jt. Settlement Status Rpt. at 1.
Borgess's opening brief to the ALJ (filed February 5, 2016) largely echoed or elaborated on points made in its request for reconsideration. Borgess contended that the Mattawan, Richland, and Three Rivers clinics met the public awareness requirement in part because information available to patients inside the clinics "presented . . . clear explanations of the [clinics'] provider-based status before those patients received care," thereby "achiev[ing] CMS's stated goal in codifying" the public awareness requirement – namely, "protecting patients from unexpected deductible and coinsurance liability." Borgess Med. Ctr. (BMC) Opening Br. to ALJ at 2, 9-11. Borgess further contended that section 413.65(d)(4), PM A-03-030, and Johns Hopkins require CMS and administrative adjudicators to consider all relevant communications when determining whether the public awareness requirement is met – including efforts made inside a facility to inform patients about its relationship to the main provider – but that CMS failed to consider such efforts in this case. Id. at 10-11, 13-17, 20. In addition, Borgess argued that its website contained information from which a person "could easily infer" the "integration" of the clinics with Borgess Medical Center. Id. at 18-19 (citing B. Ex. 18).8
In its opening brief to the ALJ (filed on the same day as Borgess's), CMS urged the ALJ to affirm its "denial of provider-based status" for the Mattawan, Richland, and Three Rivers clinics, contending that the efforts of those clinics to hold themselves out as part of Borgess Medical Center fell short of meeting the public awareness requirement. CMS Opening Br. to ALJ at 2, 16, 23-24. The public awareness requirement was not met, said CMS, because the clinics' exterior signs did not disclose to the public that the clinics were part of Borgess Medical Center and at most "suggest[ed] a secondary affiliation to either ‘Borgess Health,' the health network to which Borgess Medical Center belongs, or ‘Borgess Health Alliance,' an undefined group that also includes Borgess Medical Center." Id. at 18. CMS further argued that the Borgess Health website did not (in 2014) clearly and unequivocally identify the clinics as outpatient departments of Borgess Medical Center, but merely as the hospital's "affiliates," a term that CMS said had been "used to describe the relationship between ProMed Physicians and Borgess Health network two years before Borgess Medical Center began treating the offices as provider-based." Id. at 13, 18 (italics in original) (citing CMS Exs. 7 and 11). In addition, CMS
Page 26
asserted that the word "public" in 42 C.F.R. § 413.65(d)(4) "demonstrates that CMS expects not only Medicare beneficiaries but also the public at large to be able to discern the relationship between the hospital and its outpatient departments." Id. at 18. CMS also argued that Johns Hopkins is not controlling, in part because it applied program guidance that section 413.65(d)(4) superseded. Id. at 22-23.
One week after the parties' opening briefs were filed, CMS objected to the admission of Borgess's Exhibits 12, 13, and 14.9 Those exhibits contain photographs of what Borgess said (in its opening brief) were "altered" signs that appeared outside the Mattawan, Richland, and Three Rivers clinics "as of October 2, 2015" – signs that included the name "Borgess Medical Center" – and invoices requesting payment for the signs' design, fabrication, and installation. See BMC Opening Br. to ALJ at 8. CMS argued in its motion that the three exhibits are irrelevant because the new signs were installed five months after CMS issued the reconsidered determination – a determination that, according to CMS, addressed only the clinics' "current and historical compliance" with the public awareness requirement. CMS Obj. to B. Exs. (filed Feb. 12, 2016) at 2-3. "Even if the new signs meet the public awareness requirement[ ] at 42 C.F.R. § 413.65(d)(4)," said CMS, "at most they are evidence of compliance with that single requirement" and "do not make it more or less probable that the [clinics] were in compliance with all provider-based regulations on the date CMS rendered its reconsideration decision." Id. at 3 (internal quotation marks omitted).
In response to CMS's motion, Borgess asserted that evidence concerning the new signs was "relevant and probative to the issue presented as it illustrate[d] Borgess's continuing efforts to adhere to CMS guidance" and "provide[d] an illustration of the Hospital's historic and current compliance efforts." BMC Br. in Support of Admission of B. Exs. 12-14 (filed March 3, 2016) at 3. Borgess further stated: "Given the issue presented, comparisons of the signage are directly relevant to the parties' competing arguments regarding the requirements to be met under the Public Awareness Standard." Id.
The ALJ's Decision
Although neither party indicated in its briefs to the ALJ that October 2, 2015 – the date by which Borgess had allegedly installed redesigned signs outside the Mattawan, Richland, and Three Rivers clinics – was legally relevant, the ALJ used that date to define the compliance issues under review. The ALJ stated that those issues were: (1) whether the three clinics met the public awareness requirement "prior to" October 2, 2015 (see ALJ Decision at 7-8); and (2) whether the clinics met that requirement – and all other requirements for provider-based status – "as of" October 2, 2015 (id. at 15).
Page 27
Before addressing those issues, the ALJ overruled CMS's objection to the admission of Borgess Exhibits 12, 13, and 14, stating that they were "highly relevant to demonstrate that [Borgess] was in compliance with all requirements for provider-based status as of October 2, 2015." Id. at 3. The ALJ also stated that the ALJ was "not limited to reviewing CMS's reconsidered determination to decide whether it was in error," and was "required to conduct a de novo review of the evidence to determine if and when [Borgess] met the provider-based requirements for the three facilities in issue." Id. at 16 (italics added, citing 42 C.F.R. § 498.3(b)(2)).
Addressing the first compliance issue, the ALJ began by examining section 413.65(d)(4)'s two-sentence text. Relying on the second sentence, the ALJ held that the regulation's "plain language" provides that patients, "as they ‘enter the provider-based facility or organization,'" must be "‘aware that they are entering the main provider'" so that "they can know that they will be billed as if at the main provider's campus," and that "[i]f patients are not aware that they are entering the main provider as they enter the [allegedly provider-based] facility or organization, [then] the facility or organization does not meet the public awareness requirement." ALJ Decision at 8 (quoting 42 C.F.R. § 413.65(d)(4)) & 11. Based on that understanding of the regulation, the ALJ assessed "what a patient or the public could have known about the three [ProMed clinics] upon entering them." Id. at 8. The ALJ found that the exterior signs for the Mattawan, Richland, and Three Rivers clinics, as they appeared in CMS's August 2014 photographs, "contain no reference to ‘Borgess Medical Center'" and thus it "was not possible for the public or a patient to determine upon entering the facilities" that an individual was entering Borgess Medical Center (the ostensible main provider). Id. (citing CMS Exs. 3-5). More specifically, the ALJ found it "more likely than not that patients entering the Richland location or the Three Rivers location [in August 2014] . . . would be aware only that they were entering an office of ProMed Physicians and that the office was a part of the Borgess Health Alliance, not that they were entering a facility operated by" Borgess Medical Center, and that "patients entering the Mattawan location at best would be confused whether that location was associated with [Borgess Medical Center] or Borgess Health" given that one of that clinic's signs displayed the name "Borgess" while the sign on the clinic's door displayed the name "Borgess Health." Id. at 9 (citing CMS Ex. 3, at 1).
In addition, the ALJ:
- found that information provided or available inside a clinic would not have "give[n] a patient notice that [Borgess] was the main provider until after the patient entered, which does not satisfy the requirement of 42 C.F.R. § 413.65(d)(4)" (id. at 11-12);
- rejected Borgess's contention that the purpose of section 413.65(d)(4) is satisfied as long as patients become aware that they have entered the main
Page 28
provider "prior to receiving care," stating that section 413.65(d)(4) "clearly requires that a patient be aware upon entry of the relationship between the main provider and provider-based facility," and that "[b]ecause the regulatory language is clear, there is no need to resort to tools for interpreting that language to mean something different from what it says" (id. at 11);
- found that Borgess's evidence, including results of a consumer survey, did not permit "any inferences about what the general public or patients entering the Mattawan, the Richland, or the Three Rivers locations for treatment might think when they saw the words ‘Borgess Health' or ‘Borgess Health Alliance' on the signs for those locations, rather than ‘Borgess Medical Center'" (id. at 12-14);
- found that the content of Borgess's website has "little probative value related to the issue of whether . . . patients were aware on entering any of the three locations that those locations were operated by [Borgess]" (id. at 9); and
- held that Borgess's reliance on Johns Hopkins was "misplaced" for a number of reasons, including the fact that the decision interpreted and applied program guidance that was superseded by the applicable regulation (id. at 11-13).
Based on the foregoing findings and reasoning, the ALJ concluded that the Mattawan, Richland, and Three Rivers clinics did not meet section 413.65(d)(4)'s public awareness requirement "prior to October 2, 2015." Id. at 15.
Relying (apparently) on Borgess Exhibits 12-14, the ALJ further concluded that the clinics met the public awareness requirement "as of October 2, 2015" because, by that date, each had a new exterior sign "contain[ing] a stand-alone use of the ‘Borgess' wordmark and, more importantly, specifically list[ing] ‘Borgess Medical Center.'" Id.
Finally, the ALJ concluded that the Mattawan, Richland, and Three Rivers clinics met all other requirements (besides the public awareness requirement) for provider-based status as of October 2, 2015, and therefore the "effective date" of the clinics' provider-based status was October 2, 2015. Id. at 15-16. In support of that conclusion, the ALJ stated:
In its September 19, 2014 initial determination, CMS cited only two requirements for provider-based status that it determined [Borgess] and the Mattawan, Richland, and Three Rivers locations did not meet – 42 C.F.R. § 413.65(d)(4) and (g)(7). In its June 5, 2015 reconsidered determination, CMS determined that [Borgess] and its locations did meet the requirement of 42 C.F.R. § 413.65(g)(7), but did not meet the other, 42 C.F.R. § 413.65(d)(4). I infer from these determinations that [Borgess] and the Mattawan, Richland, and Three Rivers locations met all other applicable
Page 29
requirements for provider-based status as of the date of the reconsidered determination [June 5, 2015]. I have concluded that as of October 2, 2015, [Borgess] and the Mattawan, Richland, and Three Rivers locations met the public awareness requirement of 42 C.F.R. § 413.65(d)(4). It follows, then, that as of October 2, 2015, [Borgess] and the Mattawan, Richland, and Three Rivers locations met the requirements for provider-based status.
. . . CMS is bound by its prior initial and reconsidered determinations that strongly support the inference that CMS determined that [Borgess] met all provider-based requirements other than 42 C.F.R. § 413.65(d)(4). Thus, my conclusion that [Borgess] and the Mattawan, Richland, and Three Rivers locations have shown that they met the requirement of 42 C.F.R. § 413.65(d)(4) as of October 2, 2015, establishes that [Borgess] and the Mattawan, Richland, and Three Rivers locations met all requirements for provider-based status as of that date.
Id. at 16 (record citations omitted, italics added).
Analysis
As noted in the introduction, both parties request Board review of the ALJ's decision: Borgess appeals the ALJ's conclusion that the Mattawan, Richland, and Three Rivers clinics did not meet the public awareness requirement prior to October 2, 2015; CMS appeals the ALJ's conclusion that those clinics met the public awareness requirement, and all other applicable requirements for provider-based status, as October 2, 2015. We consider both appeals – beginning with Borgess's – under the same standard of review: we review the ALJ's findings of fact to determine if they are supported by substantial evidence, and review the ALJ's legal conclusions de novo. See Johns Hopkins, DAB No. 1712, at 2.
A. The ALJ's conclusion that the Mattawan, Richland, and Three Rivers clinics did not meet the public awareness requirement prior to October 2, 2015 is supported by substantial evidence and consistent with the governing regulation.
Borgess's request for review restates or elaborates upon arguments made before the ALJ. Although our evaluation of those arguments differs in some respects from the ALJ's, we affirm the ALJ's conclusion that the Mattawan, Richland, and Three Rivers clinics did not meet the public awareness requirement prior to October 2, 2015, because that conclusion is supported by substantial evidence and consistent with the governing regulation.
The ALJ concluded that the clinics did not meet the public awareness requirement prior to October 2, 2015 because their exterior signs at that time failed to identify the clinics as
Page 30
parts of Borgess Medical Center, the ostensible main provider. Substantial evidence supports the finding that the signs did not identify the clinics as part of Borgess Medical Center. As CMS's photographs reflect, the signs, which appeared near the clinics' entrance doors, did not include the main provider's name. In each instance, the sign identified the clinic first and foremost as "ProMed Physicians." CMS Ex. 3, at 1; CMS Ex. 4; CMS Ex. 5, at 1-3; see also CMS Ex. 8, at 1-2 (Google street views of Richland and Mattawan). Although the signs indicated, in smaller type below the ProMed Physicians name, that the clinics were part of the network of healthcare facilities known as "Borgess Health" or "Borgess Health Alliance," that information failed to convey that the clinics were parts of Borgess Medical Center because the Borgess Health network encompassed multiple types of healthcare facilities, including physician practices, not merely Borgess Medical Center.10 CMS Ex. 12.
The ALJ committed no legal error in concluding that these facts demonstrated noncompliance with the public awareness requirement. The ALJ construed section 413.65(d)(4) as requiring that a provider-based facility be identified in a way which makes patients aware "as they are entering" or "upon entering" the facility that it is part of the main provider. ALJ Decision at 8 (stating that the "regulation requires that as they enter the provider-based facility, . . . patients must be aware that they are entering the main provider" (internal quotation marks omitted)). That interpretation is not inconsistent with section 413.65(d)(4)'s second sentence, which states, as an apparent regulatory objective, that"[w]hen patients enter [a] provider-based facility or organization, they are aware they are entering the main provider . . . ." Borgess contends that the ALJ's construction of section 413.65(d)(4) "contravenes [the regulation's] plain language," B. Reply Br. at 2-3, but does not say how the ALJ's construction is incompatible with the regulation's text or specify a reasonable alternative construction that compels a conclusion different than the one the ALJ reached. The ALJ therefore did not err in concluding that the exterior signs' failure to identify the clinics as parts of Borgess Medical Center violated the public awareness requirement.
The ALJ's conclusion that the clinics did not meet the public awareness requirement is further supported by section 413.65(d)(4)'s first sentence, which states that a facility or organization meeting the public awareness requirement is one that is "held out to the public" (and to "other payers") as part of the main provider. The term "public" is commonly and ordinarily understood to mean the people or community "as a whole." Merriam Webster Online Dictionary, https://www.merriam-webster.com/dictionary/public (defining the term as the "populace" or the "people as a
Page 31
whole"); accord Black's Law Dictionary 11th ed. 2019 (defining the term as "[t]he people of a country or community as a whole"). The clinics' exterior signs, located outside and facing the surrounding community, unquestionably held out the clinics to "the public." The signs therefore had to meet the regulatory standard established in the regulation's first sentence. The signs did not meet that standard because they did not identify the clinics as part of Borgess Medical Center, the main provider.
The clinics were also not "held out to the public" on Borgess's website (Borgess.com) as being parts of Borgess Medical Center (the hospital) prior to October 2, 2015, despite Borgess's contrary claims. See B. Opening Br. to ALJ at 17 (asserting that information on Borgess.com "supplemented the Hospital's Efforts to Meet the Public Awareness Standard"). Evidence in the record shows that the website (circa 2010 and 2014), like the signs, did not meet the regulatory standard because it identified the clinics, not as integral and subordinate parts of Borgess Medical Center, but as "affiliates" or components of the "Borgess Health" network. CMS Ex. 2, at 6 (September 4, 2014 Borgess.com webpage identifying "ProMed Physicians – Family Practice" as an "affiliate of Borgess Health"); CMS Ex. 13 (Borgessnews.com webpage containing a June 2010 notice identifying the Mattawan clinic as an "affiliate" of Borgess Health).
Borgess submits that a provider-based facility "should be considered to have met the public awareness standard if, taking into account all the information provided to a patient before receiving services," including information provided inside the facility, "a beneficiary would be aware that the facility is provider-based to a main provider and understands the financial implications of that relationship." B. RR at 18-19; id. at 6 (asserting that section 413.65(d)(4) can be "interpreted rationally" to require that CMS "tak[e] account of all information available to a prospective patient, prior to the time that he or she receives services at a provider-based department"). Based on that proposition, Borgess contends that the ALJ should have found the Mattawan, Richland, and Three Rivers clinics compliant with section 413.65(d)(4) based on unrefuted evidence that, once inside the clinics, and prior to receiving services, patients received information about the clinics' "provider-based relationship" with Borgess Medical Center and the financial "implications" or consequences of that relationship. Id. at 7-8; see also B. Reply Br. at 5 (asserting that the ALJ erred in failing to consider the "plethora of information conveyed to patients in the registration area inside the Clinics and prior to receipt of services"). Those materials included: the "Important Notice" concerning Medicare billing for office visits, which states, among other things, that "Borgess Medical Center owns and operates this physician office"; the Provider-Based Medicare Billing notice indicating that a patient of the clinic would receive bills from both Borgess Medical Center and the clinic; and a treatment consent form and privacy notice, both of which bore the Borgess wordmark. B. RR at 7-8 (citing CMS Ex. 32, at 69-73). In short, Borgess contends that the clinics were compliant with the public awareness requirement prior to October 2, 2015 because, even if their exterior signs did not identify them as parts of Borgess
Page 32
Medical Center, information available or provided inside the clinics made patients aware that they had entered a part of that hospital.
We agree with Borgess that evidence about how a purportedly provider-based facility identifies itself to patients (and others) once they have entered may be probative of whether the facility meets the public awareness requirement; we disagree, however, that such evidence establishes Borgess's compliance in this case. Under Borgess's construction of section 413.65(d)(4), an off-campus provider-based facility may identify itself to the surrounding community (through exterior signage, advertising, or a website) as freestanding, or as something other than an integral and subordinate part of the main provider, but nonetheless satisfy the regulation by informing "patients" who have entered the facility that it is part of the main provider. B. Reply Br. at 3-5 (suggesting that any problems with the clinics' exterior signs are "not dispositive" if other communications "tie the facility to the main provider"); id. at 16 (alleging that information provided within its clinics helped to "clarif[y] any alleged ambiguity with the exterior signage, sufficient to meet the public awareness standard"). We see nothing in the regulation's text that permits, much less requires, the regulation to be applied in this way. If anything, Borgess's approach fails to give full effect to section 413.65(d)(4)'s first sentence, which on its face applies to any way in which a provider-based facility (or a facility that is treated as such) is "held out to the public." "The public" to whom a facility is "held out" includes not just those who enter the facility but persons outside the facility who are contemplating using its services or inquiring about available service providers, family members of patients, and others with financial or other responsibility for the care of the facility's patients. A facility treated as provider-based does not satisfy the standard in section 413.65(d)(4)'s first sentence when it identifies itself – by means intended or designed to reach the public (or "other payers") – as something other than a part of the main provider. Accepting Borgess's construction of the regulation would permit a facility to identify itself in conflicting or inconsistent ways and thereby confuse the community about its relationship to the main provider.
Borgess makes a host of other contentions or arguments, none of which persuades us that the ALJ's decision (so far as it concerns CMS's inappropriate-treatment determination under section 413.65(j)(1)) rests on prejudicial legal or factual error.11 Borgess contends that the ALJ "fail[ed] to consider" information on its website (Borgess.com) that, according to Borgess, shows that the clinics were held out to the public in accordance with section 413.65(d)(4). B. Reply Br. at 5, 6-9. The ALJ did consider the cited Borgess.com webpages but found the information on them had "little probative value"
Page 33
because there was "no evidence that any . . . patients at the Mattawan, Richland, or Three Rivers locations, check Borgess's website to learn that those locations are operated by [Borgess] so that they are aware of that fact upon entry." ALJ Decision at 9. We need not address whether that was a valid reason for discounting the website evidence because it does not help Borgess in any event. Borgess points to a webpage announcing the 2010 opening of the Mattawan clinic, emphasizing that the page's banner included the Borgess wordmark and a photograph of Borgess Medical Center.12 B. Reply Br. at 7-8 (citing B. Ex. 23). However, any impression created by the banner and photograph about the connection between Borgess Medical Center and the Mattawan clinic was muddled or obscured by the underlying announcement. The announcement identified the Mattawan clinic as "ProMed Physicians – Family Practice"; indicated that ProMed Physicians – not Borgess Medical Center – "ha[d] opened" the clinic; stated that the clinic was an "affiliate" of the Borgess Health network, not that it was a subordinate or integral part of the hospital; and explained that "Borgess Health" is a "health system" that "include[d] Borgess Medical Center," other hospitals, hospice and home health providers, and "many additional owned or affiliated services" without indicating that the Mattawan clinic was connected to any particular Borgess provider.13 B. Ex. 23. The Mattawan clinic – and the other two clinics at issue here – continued to be identified as Borgess Health "affiliates" on Borgess's website as late as September 2014.14 See CMS Ex. 7, at 1 (September 4, 2014 screenshot of Borgess.com webpage stating that "ProMed Physicians – Family Practice is an affiliate of Borgess Health" and identifying the Mattawan, Richland, and Three Rivers clinics as ProMed Physicians locations). In short, the record shows that, from 2009 through September 2014, those clinics were depicted on Borgess.com as autonomous or freestanding facilities within the Borgess Health network, rather than as integral and subordinate parts of Borgess Medical Center.
Borgess also unpersuasively argues that the signs outside the Mattawan, Richland, and Three Rivers clinics met the regulatory standard even though they did not contain the main provider's name. Emphasizing that the signs all displayed the "Borgess"
Page 34
wordmark, which it calls an "important distinctive branding tool," Borgess suggests that CMS's finding with respect to the Portage clinic that "local residents closely associate the stand-alone name ‘Borgess' with the hospital [Borgess Medical Center]" (CMS Ex. 1, at 3) applies equally to the Mattawan, Richland, and Three Rivers clinics and demonstrates that the wordmark "in isolation" informed the public that the clinics were part of Borgess Medical Center. B. Reply Br. at 9. The problem with this argument is that the signs outside the Mattawan, Richland, and Three Rivers clinics did not use the Borgess wordmark "in isolation." Rather, they used the wordmark to identify the healthcare network of which the clinics and Borgess Medical Center were a part. The argument also wrongly implies that CMS found the Borgess wordmark on the sign outside the Portage clinic to be sufficient evidence of that clinic's compliance with section 413.65(d)(4). CMS found the Portage clinic compliant based on multiple factors, including: (1) acceptance of Borgess's claim that "local residents closely associate[d]" the stand-alone name "Borgess" with Borgess Medical Center; (2) the "primary and prominent use" of the Borgess wordmark on the sign outside the clinic; and (3) "other evidence tying the [clinic] to the main provider." CMS Ex. 1, at 3. Borgess does not allege, and the evidence of record does not show, that these factors all applied equally to the other three clinics. Most notably, Borgess does not allege or cite evidence that persons living near, or otherwise likely to use, the Mattawan, Richland, and Three River clinics "closely associate[d]" the Borgess name with Borgess Medical Center in Kalamazoo. In addition, those clinics all had exterior signs that did not make "primary" and "prominent" use of the stand-alone "Borgess" name. To the contrary, and as the ALJ noted, the signs outside those clinics "muddie[d] the waters" (ALJ Decision at 14 n.6) by using the Borgess wordmark in conjunction with the words "Health" or "Health Alliance."
Borgess further contends, unpersuasively, that the ALJ's analysis – in particular, the ALJ's refusal to find the clinics compliant with the public awareness requirement based on evidence of what information patients saw or received inside the clinics – is inconsistent with PM A-03-030. See B. RR at 8-9; B. Reply Br. at 10-11. We see no inconsistency or improbability in the ALJ's interpretation of the guidance in PM A-03-030. As the ALJ noted, section 413.65(d)(4), not the program memorandum, provides the governing legal standard, and the program memorandum does not establish a relevant binding rule or purport to interpret language in the regulation. ALJ Decision at 11 ("The CMS program guidance establishes no rule, but merely provides some examples of evidence that may be considered in concluding a facility may or may not meet the public awareness requirement."). Nor does the memorandum specify any set of circumstances in which the public awareness requirement would be considered satisfied. The memorandum merely gives "examples" of "documentation" that may be "maintain[ed]" by a facility to show that the facility is "clearly identified as part of the main provider." CMS Ex. 19. Borgess seizes on one example – "patient registration forms" – implying that CMS would not have mentioned such material if information provided to patients inside the facility could not be used to demonstrate the facility's compliance with the regulation. B. Reply Br. at 11; see also B. RR at 9 ("The only way that the ALJ's
Page 35
decision could coexist with [PM A-03-030] would be for all of the provider-based facility's patient registration forms and letterhead to be made available to patients outside of the facility."). However, nothing in the program memorandum supports Borgess's implication that information provided to patients inside a facility renders that facility compliant with section 413.65(d)(4) regardless of how the facility is "held out to the public" beyond its walls. If anything, the memorandum's examples of supporting documentary evidence suggest that CMS expects any method, or all methods, used to communicate a provider-based facility's identity to the public must comply with the regulatory standard.
B. The ALJ's conclusion that the Mattawan, Richland, and Three Rivers clinics did not meet the public awareness requirement prior to October 2, 2015 is consistent with Board precedent.
Borgess contends that the ALJ's conclusion that its off-campus clinics did not meet the public awareness requirement cannot be squared with the analysis or holdings in Johns Hopkins.15 In that case, HCFA claimed that the Green Spring Oncology Center (GSOC) did not meet Criterion 7 of PM A-96-7 (the public awareness standard superseded by section 413.65(d)(4)), and thus failed to qualify as a provider-based entity of Johns Hopkins Hospital, because bills sent to GSOC's patients did not indicate that they had been sent by the Hospital and instructed that payment be made to GSOC rather than to the Hospital. DAB CR598, FFCL (Findings of Fact and Conclusions of Law) 2.d. Based on those circumstances, HCFA argued before an ALJ that patients "would not reasonably assume" that GSOC was part of the Hospital but would instead assume that it was a "separate entity." Id. The ALJ rejected that argument, reasoning that "[a]lthough the billing documents d[id] not specifically refer to the Oncology Center as being part of the Hospital, neither d[id] they state or suggest that the Oncology Center [was] an entity that [was] run separate and apart from the Hospital." Id. The ALJ also observed that the bills sent to patients referred to GSOC as "Johns Hopkins at Green Spring Station" (or "Johns Hopkins at Greenspring") and that "[a] reasonable patient could easily infer from this designation that he or she was being treated by a facility of the Hospital because both the Oncology Center and the Hospital are identified in the public mind with the prefix ‘Johns Hopkins.'" Id. In addition, the ALJ found that any ambiguity presented by the billing documents was "more than cleared up by additional information which [GSOC] and the Hospital communicated to patients."16 Id. Finally, the ALJ found that the "the manner in
Page 36
which the Hospital and [GSOC] treat[ed] . . . patients provided the[m] . . . with a clear indication that the two entities [were] wholly integrated." Id. (noting that GSOC patients were registered as patients of the Hospital, assigned Hospital identification numbers, and given a choice between receiving care at the Oncology Center or at the Hospital). The Board affirmed the ALJ's conclusion that Criterion 7 was met, finding substantial evidence that GSOC "[did] hold itself out as part of the Hospital" and noting that HCFA's analysis "fail[ed] to consider the evidence as a whole." DAB No. 1712, at 12. The Board also agreed with the ALJ that the lack of the word "Hospital" in GSOC's name was insufficient evidence of noncompliance with Criterion 7. Id.
Borgess contends that references to the Borgess Health network on signs outside the Mattawan, Richland, and Three Rivers clinics are not problematic in light of the significance attached to the hospital's name in Johns Hopkins. Borgess suggests that the Board in that case found the name "Johns Hopkins" sufficient to identify the Green Spring Oncology Center as part of Johns Hopkins Hospital (the provider). B. RR at 10 (stating that the Board "agreed" with the finding that "‘a patient could reasonably infer . . . that he or she was being treated by a facility of the Hospital because both the Oncology Center and the Hospital are identified in the public mind with the prefix ‘Johns Hopkins'" (quoting DAB CR598, FFCL 2.d)); B. Reply Br. at 10 (asserting that the ALJ in Johns Hopkins found that the Hopkins name "sufficed" to identify the oncology center as part of the hospital). Borgess submits that the Board should likewise find the "Borgess" name sufficient to identify the Mattawan, Richland, and Three Rivers clinics as parts of Borgess Medical Center, notwithstanding that name's pairing with the words "Health" or "Health Alliance." B. Reply Br. at 10.
These points omit or misstate certain details about Johns Hopkins that weaken its force as relevant precedent. As an initial matter, in our view, the names "Johns Hopkins at Greenspring" and "Johns Hopkins at Green Spring Station" are far more suggestive of a provider-based relationship than the references to the Borgess Health network on the signs outside the Mattawan, Richland, and Three Rivers clinics. Assuming that the public primarily identified the name "Johns Hopkins" with a hospital (as the ALJ in that case found), rather than with a healthcare network, the formulation "Johns Hopkins at Greenspring" or "at Green Spring Station" indicates that the hospital ("Johns Hopkins") was operating, on an inpatient or outpatient basis, "at" the named location (Greenspring). In contrast, the signs outside the Mattawan, Richland, and Three Rivers clinics do not indicate that "Borgess," the hospital, was operating at those sites, only that some parts of the Borgess Health network of facilities, namely the ProMed physician practices, were situated there.
There is also no indication that the names "Johns Hopkins at Green Spring Station" and "Johns Hopkins at Green Spring" were "advertised" (as Borgess says) to the public; those names appeared only on post-service bills sent to the oncology center's patients. In addition, contrary to Borgess's suggestion, the Board did not hold that the name "Johns
Page 37
Hopkins" was sufficient proof of compliance with the then-existing public awareness standard; the Board indicated only that, given the "longstanding association of the name ‘Johns Hopkins' with the Hospital," the "mere absence of the word Hospital'" in the facility's names (as shown on patient bills) was insufficient proof of failure by the oncology center to hold itself out as part of the hospital. DAB No. 1712, at 12. Also, the Board in Johns Hopkins acknowledged that, in the then-current "healthcare environment," the name "Johns Hopkins" referred not only to the hospital but also to the "Johns Hopkins Health Systems," creating "ambiguity" about whether a facility was part of the hospital or merely a part of the Johns Hopkins Health Systems network. Id. at 13. That ambiguity also exists with respect to the clinics at issue in this case because the record shows that the name "Borgess" was used to identify not just Borgess Medical Center in Kalamazoo, Michigan (the ostensible main provider), but other hospitals and facilities as well as a healthcare network that included Borgess Medical Center and the clinics. CMS Ex. 13, at 1 (explaining that "Borgess Health is a health system" that "includes Borgess Medical Center," other hospitals, and "many additional owned or affiliated services"); CMS Ex. 17, at 113 (notes to consolidated financial statement for the year ending June 30, 2012) (indicating that "Borgess . . . is a nonprofit health system comprising Borgess Medical Center, Lee Memorial Hospital Corporation, Promed Healthcare [and others]").
The analogy to Johns Hopkins is also weak because, unlike the provider-based facility in that case, the Mattawan, Richland, and Three Rivers clinics were prominently held out to the public under a name ("ProMed Physicians") other than the provider's. See Jt. Stip. ¶ 7 (indicating that Borgess began to treat the Mattawan clinic as provider-based in 2010, and the Richland, and Three Rivers clinics as provider-based in 2009); CMS Exs. 3-5 (the photographs showing exterior signs identifying clinics as ProMed Physicians locations); CMS Ex. 7 (September 2014 screenshot of Borgess.com webpage identifying the Mattawan, Richland, and Three Rivers clinics as ProMed Physicians: Family Practice" locations); CMS Ex. 11 (archived 2007 Borgess.com webpage listing "ProMed Physicians – Family Practice" sites in Richland and Three Rivers, Michigan). That difference is legally significant because section 413.65(d)(4), in contrast to PM A-96-7 applied in Johns Hopkins, incorporates terms – namely, "main provider" and "department of a provider" – whose definitions make it clear that a facility's provider-based status entails being operated under the name of the main provider. As defined elsewhere in section 413.65, a "main provider" is "a provider that either creates, or acquires ownership of, another entity to deliver additional health care services under its name, ownership, and financial and administrative control[.]" 42 C.F.R. § 413.65(a)(2) (italics added). And a "department of a provider" is "a facility or organization that is either created by, or acquired by, a main provider . . . under the name, ownership, and financial and administrative control of the main provider[.]" Id. (italics added). CMS asserts that section 413.65(d)(4)'s incorporation of these two terms effectively requires that a provider-based facility be held out (that is, identified) to the public using the name of the main provider. CMS's 2003 program guidance reflects CMS's view that provider-based
Page 38
sites must be "clearly identified as part of the main provider" using, among other means, a "shared name," and that "[a]dvertisements that only show the facility to be part of or affiliated with the main provider's network or healthcare system are not sufficient" to identify the facility as part of the main provider. CMS Ex. 19, at 6. We agree with CMS's interpretation of section 413.65, as it gives full meaning to terms within the regulation that otherwise would be superfluous. See Friendship Home Healthcare, Inc., DAB No. 3000, at 8 (2020) ("As a general rule, we interpret provisions in a manner that does not make any language superfluous.").
C. The ALJ Decision does not establish a new, confusing, burdensome, or unconstitutional notice requirement.
Next, Borgess contends that the ALJ effectively established a new "notice requirement" that any off-campus hospital-based facility "place signage outside" its building "advertising [it] as part of the hospital." B. RR at 14; see also id. at 17 (asserting that the ALJ "turn[ed] the public awareness standard into a positive advertising requirement"). According to Borgess, this new "notice requirement [is] more stringent than any other in the Medicare system and directly impinges upon hospitals' ability to control their operations . . . ." Id. at 14-16.
This contention is unfounded. By its terms, section 413.65(d)(4) does not mandate the posting of any signage or advertisement outside a facility or organization for which provider-based status is claimed. Instead, the regulation expressly mandates only that a facility or organization seeking provider-based status "be held out to the public and other payers as part of the main provider" so that "[w]hen patients enter the provider-based facility or organization, they are aware that they are entering the main provider and are billed accordingly." The ALJ did not hold that section 413.65(d)(4) affirmatively obligated the clinics to "place signage outside" their buildings or use specific methods to notify the public of their relationship to the main provider. The ALJ merely held that, to the extent the ProMed clinics in Mattawan, Richland, and Three Rivers advertised themselves to the public or were "held out to the public . . ." as the regulation provides, with signage, that signage needed to make the public "aware" that the clinics were part of Borgess Medical Center, the main provider.
Borgess also attributes to CMS the view that a facility treated as provider-based can meet the public awareness requirement only through "one method and one method alone" – that is, by advertising or other messaging directed at persons outside the facility. B. Reply Br. at 11. We see no indication in the record that CMS takes that view. We understand CMS's position to be that when a facility that is being treated as provider-based holds itself out to the public, the means used must clearly convey that the facility is part of the main provider. Thus, in these cases, CMS takes a position that is consistent with its own publication, PM A-03-030, which, by its terms, does not require a facility to use any particular method or a method directed to persons outside the facility. PM A-03-
Page 39
030 contemplates only that, in furtherance of holding out to the public and other payers as part of the main provider in accordance with section 413.65(d)(4), a facility "may" use any one or more means, to include "advertisements" and "signage." CMS Ex. 19, at 6. The sole express limitation PM A-03-030 imposes on the "examples" of the means listed concerns "advertisements," as it provides that "[a]dvertisements that only show the facility to be part of or affiliated with the main provider's network or healthcare system are not sufficient." Id.
Borgess further contends that the ALJ's finding that the clinics' exterior signs failed to comply with the public awareness requirement does not serve its purpose. As noted, CMS stated in the 2000 rulemaking preamble that it had promulgated section 413.65(d)(4) to help protect Medicare beneficiaries from unexpected deductible and coinsurance liability. 65 Fed. Reg. at 18,522. Borgess asserts that the ALJ's noncompliance finding does not serve that purpose unless a Medicare beneficiary would "know from seeing the [Hospital's] name outside [the] Clinic building that he or she may incur additional financial liability for the visit." B. RR at 15. Such knowledge, says Borgess, is "simply unrealistic," as "[t]he rules governing Medicare payments are . . . notoriously confusing," and "Medicare beneficiaries cannot be expected to deduce from a hospital's name the fact that they will be liable for copayments for both a professional and a facility fee." Id.
This argument, too, shows no error by the ALJ. The ALJ's finding serves the regulation's purpose – to help protect Medicare beneficiaries from unexpected deductible and coinsurance liability – because exterior signs identifying the clinics using the name Borgess Medical Center would have alerted patients (and other members of the public) to a circumstance – namely, that the clinics were operating as outpatient hospital facilities – that could affect patients' financial liability for services obtained in those facilities. It may be true, as Borgess posits, that many clinic patients would not have instantly or automatically deduced from the hospital's name on the clinics' signs that services rendered in those clinics would result in liability for a share of a "facility fee" or have other specific Medicare billing and payment consequences. But it is not implausible that awareness of the clinics' link to Borgess Medical Center might cause some patients (or their representatives), particularly those with experience in dealing with the health care system, to inquire about – or at least be more alert to – the possibility that charges for services in the clinics might be higher than they otherwise would be in a non-hospital or non-hospital-affiliated setting. In any event, Borgess's argument overlooks the purpose of the public awareness requirement, and other requirements for provider-based status, to protect not only Medicare beneficiaries but also the Medicare trust fund, by "ensur[ing] that higher levels of Medicare payment" associated with that status "are limited to situations where the facility or organization is clearly and unequivocally an integral and subordinate part of a provider." 65 Fed. Reg. at 18,506 (italics added); id. at 18,504 (citing a risk of "increasing program payments" stemming from the "fail[ure] to
Page 40
distinguish properly between provider-based and free-standing facilities or organizations").
Borgess asserts that "in no other situation does CMS require a provider to post a billing notice on the outside of its buildings," but we reject Borgess's implication that the ALJ held that the clinics could not have met the public awareness requirement unless they posted such a notice. See B. RR at 15. The ALJ recognized that CMS had found the clinics compliant with section 413.65(g)(7)'s notice requirements concerning provider-based billing. Section 413.65(g)(7) provides that when a Medicare beneficiary is treated in an off-campus hospital outpatient department, "and the beneficiary will incur a coinsurance liability for an outpatient visit to the hospital as well as for a physician service," then the hospital (that is, the main provider) must provide a "written notice" to the beneficiary, prior to service delivery, of: "(A) The amount of the beneficiary's potential financial liability; or (B) If the exact type and extent of care needed are not known, an explanation that the beneficiary will incur a coinsurance liability to the hospital that he or she would not incur if the facility were not provider-based, an estimate based on typical or average charges for visits to the facility, and a statement that the patient's actual liability will depend upon the actual services furnished by the hospital." Two of the three documents Borgess cites as evidence of compliance with the public awareness requirement – the "Important Notice" and the "Provider-Based Medicare Billing" information sheet – were also cited by Borgess as evidence of its compliance with section 413.65(g)(7). See CMS Ex. 32, at 5 (citing "Exhibit 13" to Borgess's reconsideration request). The ALJ concluded that Borgess had violated the public awareness requirement solely because the clinics' exterior signs did not identify them as parts of Borgess Medical Center. The ALJ did not identify any other basis for that conclusion, much less suggest that section 413.65(d)(4) required exterior posting of a "billing notice" (whatever Borgess means by that term).
Borgess claims that the ALJ's decision may "have the unfortunate effect in sowing confusion among providers, Medicare Administrative Contractors . . ., and the CMS Regional Offices with respect to the provider-based requirements." B. RR at 13. In support of that claim, Borgess cites a 2016 Office of Inspector General report which, according to Borgess, "‘reported challenges associated with unclear guidance from CMS regarding documentation necessary to support compliance with provider-based requirements.'" Id. (quoting from OIG Report No. OEI-04-12-00380 (June 2016), titled "CMS is Taking Steps to Improve Oversight of Provider-Based Facilities, but Vulnerabilities Remain"). Borgess submits that the ALJ's decision "may even contradict" the Office of Inspector General's understanding of what evidence is sufficient to demonstrate compliance with the public awareness requirement. Id. at 13-14.
We reject these points for two reasons. First, they are based on a report that Borgess did
Page 41
not submit or ask the Board to make part of the record.17 Second, Borgess did not cite any finding or passage in the report supporting its claim that the ALJ decision might sow confusion about the "documentation necessary" to show compliance with the public awareness requirement. Borgess admits that the OIG report "does not describe the documentation the OIG believed to be sufficient to demonstrate compliance with the public awareness standard" (B. RR at 14), undercutting its suggestion that the ALJ's decision might "contradict" the OIG's understanding of what section 413.65(d)(4) requires.
Borgess contends that the ALJ's decision "violates a basic principle of Medicare participation, i.e., that participation should not unduly burden a provider's right to run its business." B. RR at 17. According to Borgess, "hospitals choosing to participate in the Medicare program can expect that they will have to comply with regulations that CMS promulgates in the interest of patient health and safety, but they are permitted to maintain discretion over other business decisions." Id. The ALJ's decision "is wrong," Borgess says, because it will "cause CMS to control both whether and how a hospital chooses to advertise its provider-based facilities, setting limits on a hospital's control over its business decisions without a statutory basis and without creating any offsetting benefit to program beneficiaries." Id. (italics in original).
We reject this argument because it shows no error by the ALJ in applying section 413.65(d)(4) to the facts of this case. Borgess cites no statute, regulation, or CMS legal interpretation embodying the undue-burden principle it describes. The only authority Borgess cites for the principle is a sentence from CMS program guidance addressing 42 C.F.R. § 482.12, which requires that a hospital, as a condition of participation in Medicare, have an effective governing body that is legally responsible for the conduct of the hospital. B. RR at 17 (citing State Operations Manual, CMS Pub. 100-07, App. A, at A-0043, available at https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_a_hospitals.pdf). The cited sentence states (in full): "CMS defers to the governing bodies of hospitals to weigh the pertinent factors and permissible options, and to make business decisions in their best interest when applying to participate in Medicare" (italics added). The "options," "factors," and "business decisions" to which this sentence alludes concern how a hospital and its owned facilities or campuses elect to enroll in Medicare (as separately certified facilities or a single integrated hospital), and how hospitals within a group or healthcare network choose to be governed for purposes of meeting the condition of participation in 42 C.F.R. § 482.12 (for example, whether to have a single body act as governing body for multiple separately certified hospitals or to have a governing body for each separately certified hospital). The cited sentence does not purport to establish any general principle that
Page 42
Medicare program requirements applicable to an enrolled provider should not unduly constrain the provider's "business decisions."
Furthermore, the Board cannot disregard or fail to apply an otherwise applicable regulation based on extra-legal considerations, and Borgess has overlooked CMS's official position on this subject. When it promulgated section 413.65 in 2000, CMS rejected the suggestion of a commenter that requiring provider-based facilities to operate under the name of the main provider unduly interferes with, or constitutes "micromanagement" of, providers' marketing and other business decisions.18 Even if Borgess's undue-burden claim were legally relevant, we would reject it because Borgess does not allege that the challenged determinations unduly burdened its own legitimate business "discretion." Borgess merely speculates that CMS might in other circumstances rely on the ALJ's decision to unduly limit such discretion.19
Finally, Borgess suggests that the ALJ's "interpretation" or application of the public awareness requirement "may" violate the First Amendment to the Constitution because it compels Borgess to speak (i.e., "advertise") in a way that does not advance the stated purpose of the regulation. B. RR at 18. It is questionable whether we can consider the merits of this suggestion at all. In general, the Board is bound by applicable statutes and regulations and has no authority to declare them unconstitutional or fail to follow them on that ground. See, e.g., Michael Scott Edwards, OD, et al., DAB No. 2975, at 18 (2019) ("ALJs and the Board are bound by the regulations and may not declare them unconstitutional or decline to follow them on that basis." (internal quotation marks omitted)); Urology Group of NJ, LLC, DAB No. 2860, at 14 (2018) ("The Board may not declare unambiguous statutes or regulations unconstitutional and decline to follow them on that basis.").
Page 43
Even if we considered this case as falling within the Board's power to "consider a constitutional claim to the extent that it challenges the manner in which a regulation is interpreted or applied in a particular case," Urology Group at 14, we would reject Borgess's constitutional argument as unsupported. Borgess provides no supporting legal analysis and cites no pertinent caselaw. It merely cites a law review article addressing "compelled commercial speech"20 but does not indicate what, if anything, the article says about the circumstances of this case or demonstrate any error by the ALJ.
D. The ALJ's effective-date determination must be vacated.
We now turn to CMS's appeal, which concerns the ALJ's determination that the Mattawan, Richland, and Three Rivers clinics met all requirements for provider-based status, including the public awareness requirement, as of October 2, 2015 (four months after CMS issued the reconsidered determination) and that October 2, 2015 was therefore the "effective date" of the clinics' provider-based status under 42 C.F.R. § 413.65(o). (We refer to that determination as the ALJ's "effective-date determination.")
CMS contends that the ALJ's effective-date determination "exceeded the permissible scope of de novo review." CMS Request for Review (CMS RR) at 1, 21-22. CMS submits that the only adverse determination appealed to the ALJ was an inappropriate-treatment determination under 42 C.F.R. § 413.65(j)(1); that an inappropriate-treatment determination and an effective-date determination under section 413.65(o) are "two different administrative actions that arise under different sections of the provider-based rule"; and that the "ALJ had no authority to determine an effective date [of the clinics' provider-based status] as a matter of first impression." Id. at 1, 10-11, 14 n.5, 19-22 (asserting that by determining the clinics' effective date of provider-based status, the ALJ "supplant[ed] CMS's ability to make initial determinations as to provider-based status in accordance with the regulations"). CMS further contends that the ALJ's effective-date determination is substantively "erroneous." Id. at 16-19, 22-23. Borgess responds that the clinics' post-reconsideration entitlement to provider-based status was "appropriately before" the ALJ and asks us to affirm the ALJ's effective-date determination. B. Response Br. at 6-18.
We conclude that the effective-date determination must be vacated for at least three reasons. First, the clinics' post-reconsideration entitlement to provider-based status was a matter that the regulations authorized CMS to address in the first instance, and the ALJ provided no valid reason for preempting CMS's exercise of that authority. Second, putting aside for the moment our determination that the ALJ improperly reached and decided the clinics' prospective entitlement to provider-based status, in making an
Page 44
effective-date determination, the ALJ addressed a matter about which the parties had not expressed any disagreement, and did so without advance notice to them. Third, even if the clinics' prospective entitlement to provider-based status was a matter properly before the ALJ, the ALJ's effective-date determination cannot stand because the finding upon which it rests – that the Mattawan, Richland, and Three Rivers clinics met all requirements for provider-based status as of October 2, 2015 – is not supported by substantial evidence.
- The ALJ stated no valid reason for making a determination that the regulations authorized CMS to make in the first instance.
As noted, under 42 C.F.R. § 413.65, a provider may treat an off-campus subordinate facility as provider-based, without having first sought a determination (by CMS) of provider-based status, but at the risk of certain specified consequences if CMS later determines under section 413.65(j)(1) that the facility in fact "did not meet" one or more requirements for provider-based status. As specified elsewhere in section 413.65(j), when CMS finds that a provider has inappropriately treated a facility as provider-based, CMS adjusts "future payments" for that facility's services to reflect the amount paid to a freestanding facility. 42 C.F.R. § 413.65(j)(3), (j)(4). Also, if the provider provides timely notice that it intends to establish the facility's status as either provider-based or freestanding, CMS allows Medicare payments for the facility's services to continue (at the adjusted rate) for up to six months during which the provider may attempt to establish that status. Id. § 413.65(j)(5); see also 67 Fed. Reg. at 50,092-93 (indicating that continued payment at the adjusted rate is appropriate "to allow for an orderly transition to either provider-based or freestanding status for the facility and to avoid disruption in the delivery of services to patients, particularly Medicare patients"). Section 413.65 further provides that CMS "will not treat," as provider-based, a facility that was inappropriately treated as such until two things occur: (1) the provider submits to CMS a "complete request for a determination" of the facility's provider-based status and any "other information needed by CMS" to make that determination (42 C.F.R. § 413.65(j)(5)(iii)); and (2) CMS determines – "based on documentation submitted by the provider" – a date upon which the facility "meets all requirements" for provider-based status (id. § 413.65(o)(2)). See also id. § 413.65(j)(5)(v) (providing that, "[i]f the necessary applications or information are not provided," then CMS "will terminate all payment" with respect to a facility that has been inappropriately treated as provider-based "as of the date CMS issues notice that necessary applications or information have not been submitted").
Having determined that Borgess inappropriately treated the Mattawan, Richland, and Three Rivers clinics as provider-based, CMS took several actions in accordance with section 413.65(j). CMS's September 19, 2014 initial determination and June 8, 2015 letter informed Borgess that if it wished to treat those clinics as provider-based, it needed to submit a complete request for CMS determination of whether the clinics were "in
Page 45
compliance with all of the provider-based requirements and obligations." B. Ex. 19, at 1 (instructing Borgess to submit "complete attestations of provider-based status" if it wished to treat the clinics as "provider-based departments of Borgess Medical Center"); CMS Ex. 2, at 3 (instructing Borgess to submit a "complete request for a provider-based determination" within 90 days). CMS further informed Borgess that if it did not file such a request (or an application to enroll the clinics in Medicare as freestanding physician practices), then CMS would terminate all payments with respect to the clinics' services "as of the date CMS issues notice that necessary applications or information has not been submitted." CMS Ex. 2, at 3. In addition, CMS advised that it would determine the clinics' provider-based status "only upon review of the attestation and any associated material." B. Ex. 19, at 1. Although Borgess notified CMS in November 2014 that it had elected "Option 1" in the initial determination – which allowed Borgess the opportunity to "make the changes needed for [the clinics] to comply with the provider-based rules" and to "seek a determination of provider-based status" for the clinics (see CMS Ex. 2, at 3, and CMS Ex. 31) – there is no evidence that Borgess has requested a determination by CMS of the clinics' post-reconsideration entitlement to provider-based status or that CMS has made an adverse determination concerning that status. The only matter addressed in the reconsidered determination, and the only matter appealed to the ALJ, was whether Borgess had inappropriately treated the clinics as provider-based on account of their failure to meet the public awareness requirement. See July 31, 2015 Request for Hearing at 2 (stating that Borgess was appealing the portions of the reconsidered determination classified as "unfavorable").
Given these circumstances – especially Borgess's choice not to use the regulation-specified, CMS-directed process for clarifying the clinics' Medicare program status – it was improper, or at least premature, for the ALJ to determine an effective date of the clinics' provider-based status. Cf. Farzana Naqvi M.D., et al., DAB No. 3016, at 1, 7-8 (2020) (holding that it was improper for the ALJ to address, sua sponte, the Medicare supplier's entitlement to a period of retrospective Medicare billing when the reconsidered determination being appealed did not address that matter).
The ALJ suggested that the administrative appeal regulations in 42 C.F.R. Part 498 "required [the ALJ] to conduct a de novo review of the evidence" to make an effective-date determination, ALJ Decision at 16 (italics added), but that is incorrect. No such obligation arose under those regulations because CMS had not issued an appealable adverse determination addressing the clinics' post-reconsideration entitlement to provider-based status. See 42 C.F.R. §§ 498.3(b)(2) (identifying, as an appealable matter, an initial determination without respect to "[w]hether a prospective department of a provider . . . qualifies for provider-based status") and 498.5 (providing hearing rights with respect to initial or reconsidered determinations issued by CMS or the Office of Inspector General); Columbus Park Nursing & Rehab. Ctr ., DAB No. 2316, at 6 (2010) (holding that a provider had a right to a hearing before an administrative law judge when
Page 46
CMS has "made an adverse ‘initial determination' of a kind specified in 42 C.F.R. § 498.3(b)").
The ALJ also held that CMS had relinquished its authority to make an effective-date determination concerning the Mattawan, Richland, and Three Rivers clinics. As the predicate for that holding, the ALJ suggested that, upon notifying Borgess on June 8, 2015 that proposed changes to the clinics' exterior signs appeared compatible with the public awareness requirement (see B. Ex. 19), CMS should have reopened and revised the June 5, 2015 reconsidered determination "within the 12-month window" in accordance with 42 C.F.R. § 498.30 in order to determine an effective date of the clinics' provider-based status. ALJ Decision at 16 n.7. By not doing so, said the ALJ, CMS "effectively waived the opportunity" to decide whether the clinics were compliant with the provider-based status requirements as of October 2, 2015, thereby "leaving the issue to me for resolution." Id.
We disagree with that holding for at least two reasons. First, it incorrectly assumes that two different determinations are conjoined and must be resolved together: the determination that a provider has inappropriately treated a facility as provider-based, and an effective-date determination with respect to that facility. As our description of the regulatory scheme makes clear, those two determinations are legally distinct and temporally separate. An inappropriate-treatment determination under section 413.65(j)(1) addresses whether a facility that a provider was treating as provider-based, and for which a provider has not requested a determination of entitlement to provider-based status, did not meet one or more requirements for that status. On the other hand, an effective-date determination under section 413.65(o)(2) is based on a request, filed after CMS notifies the provider of the inappropriate-treatment determination, that CMS determine the facility's entitlement to provider-based status. Such a determination reflects an assessment of whether the facility meets "all requirements" for provider-based status, not just the requirement(s) addressed in the underlying inappropriate-treatment determination.
Second, contrary to Borgess's suggestion, CMS had no "opportunity" to determine the clinics' entitlement to provider-based status. That opportunity could not have arisen until Borgess complied with CMS's instructions (in both the initial determination and CMS's June 8, 2015 letter) to submit a "complete" request for a determination of the clinics' provider-based status. As indicated, there is no allegation or evidence that Borgess submitted such a request, either within the one-year reopening period or later. And the regulations did not obligate CMS to make an effective-date determination until Borgess asked it to do so.
In another bid to justify the ALJ's effective-date determination, Borgess asserts that "the regulations compel an ALJ" to determine a facility's effective date of provider-based status "where possible" so that the main provider is not left "in a procedural limbo." B.
Page 47
Response Br. at 10-15 (italics added). According to Borgess, under CMS's application of sections 413.65(j) and 413.65(o), the main provider is forced to make an "untenable" choice:
[A] provider [must] either adopt changes at the provider-based sites to bring them in line with CMS's potentially flawed interpretation of the provider-based regulations, then submit a complete request for determination of provider-based status or, in the alternative, submit a request for determination without correcting the purported issue and appeal from a decision that would inevitably find that the site was not in compliance with the regulations. The former option could require the provider to expend significant resources complying with an incorrect interpretation of the regulations, including making expensive alterations to the facilities' physical plant or disrupting existing provider relationships to the detriment of patients. And under the latter interpretation, the provider could lose the ability to bill for services provided at the site during the pendency of the duplicative appeals. 42 C.F.R. § 413.65(j)(5)(v) (requiring CMS to terminate a purported provider-based site when the provider does not provide information that CMS considers sufficient to demonstrate compliance with the provider-based regulations).
Id. at 13. Borgess suggests that an ALJ should be allowed to make an effective-date determination as part of any appeal of an inappropriate-treatment determination so that the provider will not have to make the choice just described.
This argument amounts to a claim that a provider that has inappropriately treated a facility as provider-based may use the administrative appeal process in 42 C.F.R. Part 498 to establish the facility's entitlement to provider-based status in lieu of the process described in section 413.65(j). We see nothing in section 413.65 or the Part 498 regulations permitting the section 413.65(j) process to be bypassed in this way. Moreover, Borgess does not claim that it faced the "untenable" choice it describes, indicating that it pursued a "middle path." See B. Response Br. at 10-11. Indeed, Borgess is silent about why it did not seek provider-based status for the Mattawan, Richland, and Three Rivers clinics using the process that section 413.65(j) and CMS afforded.
In any event, the "untenable" choice posited by Borgess arises only if a main provider disagrees with an inappropriate-treatment determination and wants to obtain provider-based status for the affected facility without having to remedy the noncompliance identified by that determination, which is not the posture Borgess took in this case. Borgess disagreed with, and appealed, the inappropriate-treatment determination concerning the Mattawan, Richland, and Three Rivers clinics, and claimed to have taken prompt action to address the findings in that determination, yet (inexplicably) failed to
Page 48
follow through on its stated intent to seek provider-based status for the clinics. We see nothing improper about requiring a Medicare provider to choose between complying with CMS's interpretation of provider-based status requirements, and foregoing provider-based billing while challenging that determination.
- The parties did not ask the ALJ to decide whether, and if so when, the clinics became entitled to provider-based status after June 5, 2015 (the date of the reconsidered determination), and the ALJ did not notify the parties in advance that the ALJ Decision would address that matter.
The ALJ Decision rendered an effective-date determination even though the parties' briefs and other material did not identify a dispute about the affected clinics' post-reconsideration entitlement to provider-based status, and even though the ALJ did not notify the parties in advance that the ALJ intended to determine the effective date of that status. In our view, the ALJ's omission violated an "essential requirement" of the administrative appeal regulations in 42 C.F.R. Part 498 that "parties be afforded written notice of issues to be resolved by the ALJ." Kaulson Laboratories, Inc., DAB No. 1747, at 11 (2000); see also 42 C.F.R. §§ 498.47(a) (providing that a prehearing conference's purposes include "delineating the issues in controversy"), 498.50(b)(1) (providing that an order setting forth the results of a prehearing conference should be sent to the parties prior to the hearing, and indicate "the matters to be considered at the hearing, and the issues to be resolved"), and 498.52(b) (providing that a notice of hearing will "inform[ ] the parties of the general and specific issues to be resolved at the hearing").
Borgess argues that the parties identified a dispute about the clinics' post-reconsideration entitlement to provider-based status in their Statement of Issues Presented (Joint Statement). That submission states that the compliance issue to be resolved was "whether each of the three off-campus ProMed Physicians Family Practice locations [i.e., Mattawan, Richland, and Three Rivers clinics] meets the requirements to qualify as provider-based to the main provider, Borgess Medical Center" (italics added). Borgess contends that the present-tense phrase "meets the requirements" connotes "both past and present compliance" and "clearly shows that the parties sought the ALJ's determination as to whether and when the [clinics] came into compliance with the provider-based regulations" after the date of the reconsidered determination. B. Response Br. at 5-7.
We do not agree that the Joint Statement "clearly" requested such a determination, in part because it does not allude to any disagreement about when (after June 5, 2015) the clinics were, or became, entitled to provider-based status. Borgess asserts that the ALJ "relied on the stipulated issue statement" (referring to the Joint Statement) and took that statement at "face value" when he "stat[ed] that the issue for him to decide was whether the [clinics] ‘meet requirements for provider-based status.'" B. Response Br. at 8 (quoting ALJ Decision at 3). However, the ALJ did not cite the Joint Statement as
Page 49
justification for making the effective-date determination or find that the parties had asked the ALJ to make that determination.
Nothing else in the hearing record indicates that the clinics' effective date of provider-based status was at issue. The parties' briefs to the ALJ addressed the validity of the inappropriate-treatment determination – more specifically, whether the Mattawan, Richland, and Three Rivers clinics met the public awareness requirement before or on the date of that determination. See, e.g., B. Opening Br. to ALJ at 9-12, 15-20; B. Reply Br. to ALJ at 2-10. Those briefs contained no request that the ALJ render an effective-date determination. In addition, Borgess did not implicitly seek an effective-date determination by claiming that the clinics had met all requirements for provider-based status as of October 2, 2015, or as of any other date. The parties' proposed findings of fact and conclusions of law likewise gave no hint that they were seeking or expecting such a determination. See, e.g., B. Proposed Findings of Fact and Conclusions of Law (submitted Feb. 5, 2016) at 6 (stating that "CMS erroneously terminated provider-based status for [the Mattawan, Richland, and Three Rivers] clinics" without further stating that the clinics became entitled to that status after the date of the reconsidered determination).
Borgess contends that CMS "conceded" in its reply brief to the ALJ that the effective-date issue was "properly before the ALJ," B. Response Br. at 6, 8, but no such concession is apparent. The only portion of the reply brief cited by Borgess is CMS's concluding request that the ALJ find that the clinics "‘do not meet the provider-based status requirements'" – the same ambiguous, inconclusive phrasing that appears in the Joint Statement. Id. at 6 (italics added) (citing CMS Reply Br. to ALJ at 18). Furthermore, CMS argued to exclude evidence (Borgess Exhibits 12-14) that Borgess had installed new signs in early October 2015 as irrelevant to deciding what CMS evidently thought was the only matter under review – namely, the validity of the inappropriate-treatment determination. CMS Reply Br. to ALJ at 10 n.1 (stating that "even if the new signs meet the public awareness requirements at 42 C.F.R. § 413.65(d)(4), at most they would be evidence of compliance with that one requirement and no earlier than the installation date, which cannot show error with CMS's determination on review here") (italics added). CMS maintains on appeal that the ALJ admitted that irrelevant evidence in error. See CMS RR at 16-18.21 These procedural facts undercut the notion that CMS consented to the ALJ's effective-date determination.
Borgess further suggests that the ALJ's effective-date determination resolved a "new issue" that the ALJ had authority to entertain under 42 C.F.R. § 498.56. B. Response Br.
Page 50
at 16. In relevant part, section 498.56 states that, within certain time limits (not applicable to this case), and except for provider or supplier enrollment appeals, "the ALJ may, at the request of either party, or on his or her own motion, provide a hearing on new issues that impinge on the rights of the affected party . . . even if CMS . . . has not made initial or reconsidered determinations on them, and even if they arose after the request for hearing was filed or after the prehearing conference." 42 C.F.R. § 498.56(a)(1)-(2).
We decline to consider whether section 498.56 permitted the ALJ to treat the effective date of the clinics' provider-based status as a "new issue" because the ALJ did not in fact do so. Even assuming that section 498.56 authorized the ALJ to decide the effective-date issue, the ALJ could not have fairly done so without first giving the parties notice and an opportunity for a hearing on the matter. See 42 C.F.R. §§ 498.56(a)(1) (authorizing the ALJ to "provide a hearing on new issues that impinge on the rights of the affected party (italics added)) and 498.56(c)(1) (providing that "notice of the time and place of hearing on any new issue will be given to the parties in accordance with § 498.52"); see also Jennifer Matthew Nursing & Rehab. Ctr., DAB No. 2192, at 49 (2008) (observing that section 498.56 "authorizes an ALJ to add new issues, on her own motion, so long as he/she gives notice in accordance with sections 498.56(c) and 498.52"); Meadowwood Nursing Ctr., Ruling No. 2014-1 (on Petition for Reopening of DAB No. 2541 (2013)), at 8 (citing 42 C.F.R. § 498.56 and noting that CMS may raise "new issues" not addressed in the underlying agency determination so long as the provider has "adequate notice and an opportunity to respond").
- The ALJ's finding that the clinics met all requirements for provider-based status as of October 2, 2015 is not supported by substantial evidence.
Regardless of our other holdings, and even assuming for the moment the ALJ properly addressed the effective-date issue, the ALJ's conclusion on that issue cannot stand because it is not supported by substantial evidence. The ALJ found the Mattawan, Richland, and Three Rivers clinics were entitled to provider-based status as of October 2, 2015 because they "met all requirements" for that status on that date. ALJ Decision at 2. However, the ALJ could not find the clinics entitled to provider-based status – as off-campus departments of Borgess Medical Center – absent evidence of their compliance with requirements in subsections (d) and (e) of section 413.65 relating to licensure (413.65(d)(1)), clinical services (413.65(d)(2)), financial integration (413.65(d)(3)), public awareness (413.65(d)(4)), ownership and control (413.65(e)(1)), administration and supervision (413.65(e)(2)), and location (413.65(e)(3)). See 42 C.F.R. § 413.65(d) (stating that "[a]ny facility . . . for which provider-based status is sought . . . must meet all requirements" in subsection (d)); id. § 413.65(e) (specifying "additional requirements" for provider-based status applicable to "off-campus" facilities). The clinics also had to satisfy various requirements in subsection (g) in order "[t]o qualify for provider-based status in relation to a hospital." Id. § 413.65(g) (specifying requirements "[t]o qualify for
Page 51
provider-based status in relation to a hospital"). Except with respect to the public awareness requirement in section 413.65(d)(4) and the notice-of-coinsurance-liability requirement in section 413.65(g)(7), there is no evidence in the record of the clinics' compliance with the requirements for provider-based status in sections 413.65(d), 413.65(e), and 413.65(g).
The ALJ reached the effective-date holding by inferring from the initial and reconsidered determinations that CMS had found the Mattawan, Richland, and Three Rivers clinics compliant with "all provider-based requirements" except for the public awareness requirement. ALJ Decision at 16. Based on that inference, the ALJ held that it was unnecessary for Borgess to submit evidence of compliance with any applicable requirement (other than section 413.65(d)(4)). Id.
We reject that holding as based on an unreasonable inference. See Barry D. Garfinkel, M.D., DAB No. 1572, at 6 (1996) ("The substantial evidence standard does not require us to treat every inference an ALJ draws from the evidence as per se reasonable. . . ."), aff'd, Garfinkel v. Shalala, No. 3-96-604 (D. Minn. June 25, 1997). The ALJ's inference is unreasonable because nothing in the initial or reconsidered determinations, or in any other document of record, suggests that CMS's 2014 compliance investigation, triggered by a patient billing complaint, involved an assessment of the clinics' compliance with any requirements besides the two that were addressed in those determinations (and which the billing complaint directly implicated). See id. (emphasizing that, although the Board generally accords considerable deference to an ALJ's judgment in weighing the evidence and assessing witness credibility, "the ALJ's judgment must be supported by reliable, credible evidence in the record").
In addition, the ALJ's inference cannot be squared with the initial determination's instructions to Borgess about the steps it needed to take before CMS would treat the clinics as provider-based. In accordance with section 413.65(j)(5), the initial determination advised Borgess that CMS would not recognize the clinics as provider-based unless Borgess submitted a "complete request . . . for a provider-based determination." CMS Ex. 2, at 3. The demand for a "complete" request for provider-based status clearly implies that CMS had not assessed the clinics' compliance with requirements other than the public awareness and notice-of-coinsurance liability requirements, the only two requirements mentioned in the initial determination. A finding that the clinics met other applicable requirements (relating to licensure, clinical services, financial integration, ownership and control, etc.) would have been impossible without supporting documentation from Borgess – documentation it does not claim to have provided to CMS during the 2014 compliance investigation and did not provide in its reconsideration request. See, e.g., B. Ex. 10, ¶ 15 (asserting that "[h]ospitals are not required to submit an attestation or any other documentation to begin billing a site as provider-based," and that Borgess "did not do so for the" clinics at issue in the case); B. Ex. 32 (request for reconsideration).
Page 52
The ALJ's inference is also unreasonable in light of CMS's June 8, 2015 letter, sent three days after CMS issued the reconsidered determination. Like the initial determination, the June 8th letter clearly implied that CMS had not yet assessed the clinics' compliance with any requirements other than the ones pertaining to public awareness and coinsurance liability, because CMS's letter reminded Borgess that if it wished to treat the Mattawan, Richland, and Three Rivers clinics as provider-based, it needed to "submit complete attestations of provider-based status for each facility." B. Ex. 19, at 1. The letter further cautioned that CMS would determine the clinics' entitlement to provider-based status "only upon review of" a submitted attestation and supporting material. Id. The June 8, 2015 letter's information requests and warnings would have been meaningless if CMS already had the necessary materials and had made the provider-based status determination.
Borgess suggests that allowing the clinics to resume provider-based billing as of October 2, 2015 based solely on evidence of compliance with the public awareness and notice-of-coinsurance liability requirements would be consistent with CMS's treatment of the Portage clinic. Borgess claims that the Portage clinic was allowed to continue such billing after CMS found it compliant with those requirements at the reconsideration level. B. Response Br. at 15 (asserting that the ALJ's effective-date determination "aligns with" CMS's approach to the Portage clinic, which, after the reconsidered determination, was "permitted to bill as provider-based without proving compliance with any other provider-based requirements").
Borgess's suggestion overlooks the fact that the Mattawan, Richland, and Three Rivers clinics were not in the same legal position as the Portage clinic was after the reconsidered determination. CMS upheld its initial determination that Borgess had inappropriately treated the Mattawan, Richland, and Three Rivers clinics as provider-based, so those clinics were subject to provisions in section 413.65(j) that effectively disentitled them to Medicare payment as provider-based facilities unless and until Borgess asked CMS to determine their entitlement to provider-based status and CMS acted favorably on that request. In contrast, CMS reversed its initial determination that the Portage clinic had been inappropriately treated as provider-based, returning that clinic to the status quo prior to the initial determination, and so that clinic was not subject to the provisions in section 413.65(j) and could continue to bill its services as provider-based without a determination by CMS of its entitlement to provider-based status.
- Borgess's other contentions fail to establish the validity of the ALJ's effective-date determination.
Borgess's other defenses of the ALJ's effective-date determination are unpersuasive. Borgess suggests that CMS's appeal is based on "an unreasonably draconian interpretation of a conflicting set of regulations." B. Response Br. at 15. However, Borgess is unclear about what regulations it thinks are in conflict, or how CMS is
Page 53
unreasonably interpreting or applying them to support its appeal. As outlined above, CMS has identified multiple valid grounds for vacating the ALJ's effective-date determination.
Borgess also attempts to submit new evidence in support of arguments involving acquiescence and waiver. Borgess asserts that, in the process of recouping Medicare overpayments stemming from the provider-based billing of services furnished by the Mattawan, Richland, and Three Rivers clinics prior to October 2015, CMS "acquiesced to accept the changes that Borgess made [to the clinics' signs] in October 2015 as sufficient evidence of compliance with the Public Awareness Requirement and eligibility for provider-based status." B. Response Br. at 9-10. In support of that claim, Borgess asks the Board to admit a declaration by Borgess Health's Controller, with exhibits to the declaration that include 2016-2017 correspondence between Borgess (or its counsel) and a Cost Report Audit Supervisor with Wisconsin Physicians Service (WPS), a CMS contractor. Id.
We do not admit the additional evidence. The appeal regulations provide that the Board "may" admit evidence that was not presented to the ALJ if the additional evidence is "relevant and material" to an issue before it. 42 C.F.R. § 498.86(a). However, section 498.86(a) "is permissive and does not require the Board to admit additional evidence, even if it is material and relevant." Batavia Nursing & Convalescent Ctr., DAB No. 1904, at 18 (2004), aff'd sub nom. Batavia Nursing & Convalescent Ctr. v. Thompson, 129 F. App'x 181 (6th Cir. 2005) (per curiam). In deciding whether to admit additional evidence, the Board considers whether that evidence's proponent has shown "good cause" for not producing it during the ALJ proceeding. Cmty. Nursing Home, DAB No. 1807, at 28 (2002). We need not determine whether Borgess has shown good cause for not producing the new evidence earlier. Even assuming Borgess has shown good cause to submit new evidence to the Board, Borgess proffers the evidence only as support for its arguments about acquiescence and waiver relevant to an effective-date issue that was not before the ALJ and is not for the Board to decide in these appeals. Borgess has not persuasively established that the new evidence is relevant and material to an issue that is properly before the Board. We therefore do not admit the new evidence.
Furthermore, even if we were to admit and consider this evidence, we see nothing in these materials indicating that CMS "accepted" the October 2015 changes to the clinics' signs as sufficient to establish the clinics' entitlement to provider-based status. The correspondence mainly concerned the accuracy or supportability of WPS's Medicare overpayment calculations. The correspondence does not state CMS's position regarding the clinics' entitlement to provider-based status (assuming it had one at that point), or indicate that the WPS Cost Report Audit Supervisor with whom Borgess corresponded had any authority to communicate that position.
Page 54
Relying on the same evidence, Borgess asserts a waiver argument. Borgess alleges that it informed WPS in May 2016 that Borgess continued to bill the clinics' services as provider-based after October 2015, yet CMS "did not seek to recover any purported overpayment for services rendered after October 2015." B. Response Br. at 10. Borgess also alleges that CMS did not take all of the remedial steps called for in section 413.65(j) after determining that the clinics had been inappropriately treated as provider-based. Id. at 9. Borgess asserts that "CMS is supposed to take four concrete steps" when it makes an inappropriate-treatment determination under section 413.65(j)(1), namely: (1) notify the main provider of the noncompliance and remedial consequences; (2) recover any Medicare overpayments for the time period during which the provider's subordinate facility was inappropriately treated as provider-based; (3) adjust future payments to the main provider or the subordinate facility to "estimate the amounts that would be paid for the same services in a freestanding facility"; and (4) terminate adjusted payments to the facility after six months if the provider fails to request a determination by CMS of the facility's provider-based status or to submit information required by CMS. B. Response Br. at 9 (citing or referring to provisions in section 413.65(j)(1)(i)-(ii), (j)(3), (j)(4), (j)(5)(iii), and (j)(5)(v)). Borgess alleges that CMS has completed only the first two steps with respect to the three clinics at issue. Id. Based on these allegations, Borgess contends that CMS "has waived its right to require [it] to submit a full request for provider-based status for the [Mattawan, Richland, and Three Rivers clinics]." Id. at 10.
However, Borgess does not explain how or why the purported waiver should affect our review of the ALJ's decision.22 If Borgess is suggesting that CMS waived its right under 42 C.F.R. Part 498 to appeal the ALJ's effective-date determination, we reject that proposition because there is no evidence that CMS voluntarily and knowingly gave up that right. Rehabilitation Ctr. at Hollywood Hills, DAB No. 3052, at 13 (2021) (holding that waiver is the "voluntary, intentional relinquishment of a known right" (internal quotation marks omitted)). If Borgess is asking the Board to bar CMS from attempting to ascertain the clinics' post-reconsideration entitlement to provider-based status, we deny that request too. We are unaware of any statute or regulation authorizing the Board to preclude CMS action or determinations about a matter within CMS's purview, such as the status of a Medicare provider's compliance with the provider-based rules in 42 C.F.R. § 413.65. Our authority in this appeal extends no further than reviewing whether the ALJ did or did not err in determining whether the clinics met the public awareness requirement in section 413.65(d)(4) at the time of CMS's reconsidered determination.
Page 55
Finally, Borgess asserts that if the ALJ's effective-date determination is vacated, the Mattawan, Richland, and Three Rivers clinics will be "at risk" of being terminated from the Medicare program. B. Response Br. at 14-15. Borgess asks the Board to uphold the ALJ's determination in order to remove any "uncertainty" about the clinics' Medicare-program status as of October 2, 2015. Id. at 15. We deny that request. We cannot affirm an unsupported provider-based-status determination on the ground that doing otherwise might have adverse collateral consequences for the affected provider. To the extent there is "uncertainty" about the clinics' status with the Medicare program, Borgess caused or contributed to that uncertainty by not requesting and securing a determination of the clinics' provider-based status, as CMS invited Borgess to do in 2015.
- Remanding the case is not necessary or appropriate.
Although we determine that a portion of the ALJ's decision must be vacated, we do not remand the case to the ALJ because Borgess has not identified any unresolved factual disputes relevant to our review of the ALJ's conclusion that the Mattawan, Richland, and Three Rivers clinics did not meet the public awareness requirement. Under similar circumstances, the Board has held a remand to be unnecessary. Golden Living Ctr. – Riverchase, DAB No. 2314, at 19 n.10, 23 (2010) (explaining, in decision partially affirming and partially reversing ALJ's conclusions, that Board would "issue a decision rather than remand, largely because the evidence of record is undisputed in any material respect, and no additional fact finding is required"), aff'd sub nom. Golden Living Ctr. – Riverchase v. U.S. Dep't of Health & Hum. Servs., 429 F. App'x 895 (11th Cir. 2011) (per curiam). We also note again that neither party asked the ALJ to make an effective-date determination under 42 C.F.R. § 413.65(o), or asked the Board to remand the case in the event the Board vacated that determination.
Page 56
Conclusion
We AFFIRM the ALJ's conclusion that the Mattawan, Richland, and Three Rivers clinics did not meet the public awareness requirement in 42 C.F.R. § 413.65(d)(4) prior to October 2, 2015.
We VACATE the ALJ's conclusion that the Mattawan, Richland, and Three Rivers clinics met all provider-based status requirements as of October 2, 2015.
Christopher S. Randolph Board Member
Kathleen E. Wherthey Board Member
Susan S. Yim Presiding Board Member
- 1
The hospital was called "Borgess Medical Center" when the parties' dispute arose, and so this decision will refer to it by that name. According to its website, the hospital's current name is Ascension Borgess Hospital (https://healthcare.ascension.org/en/locations/michigan/mikal/kalamazoo-ascension-borgess-hospital).
- 2
Section 603 of the Bipartisan Budget Act of 2015 (Pub. L. No. 114-74, 129 Stat. 584, 597-598), codified in section 1833(t) of the Act, prohibits Medicare outpatient hospital payment for certain services provided in newly established off-campus departments of a hospital, and requires that payment for such services be made "under the applicable [non-hospital] payment system," which CMS has determined to be the Medicare Physician Fee Schedule. See 42 U.S.C. § 1395l(t)(1)(B)(v), 1395l(t)(21)(C); 81 Fed. Reg. 79,562, 79,570, 79,699, 79,708 (Nov. 14, 2016). An off-campus department of a hospital that was engaged in outpatient hospital billing for its services prior to November 2, 2015 (the date of section 603's enactment) is exempt from section 603's payment prohibition. 42 U.S.C. § 1395l(t)(21)(B)(ii); 81 Fed. Reg. at 79,700, 79,703.
- 3
In 2018, CMS issued a final rule to reduce the disparity between Medicare payment for certain types of outpatient clinic services furnished in off-campus hospital departments (and billed as outpatient hospital services), and Medicare payment for comparable services furnished in freestanding facilities. See 83 Fed. Reg. 58,818, 58,822, 59,004-15 (Nov. 21, 2018); American Hosp. Assoc. v. Azar, 964 F.3d 1230 (D.C. Cir. 2020) (rejecting a challenge to the final rule).
- 4
Additional requirements – including those relating to ownership and control, administration, and supervision – apply to "off-campus" facilities or organizations (located apart from the provider's "campus") and hospital outpatient departments and hospital-based entities. See 42 C.F.R. § 413.65(d)(5), (e), (g); id. § 413.65(a)(2) (defining "campus").
- 5
Section 413.65(d)(4) superseded the following provision in PM A-96-7: "The entity [seeking designation as part of the provider for Medicare payment purposes] is held out to the public as part of the provider where it is based (e.g., patients know they are entering the provider and will be billed accordingly)." CMS Ex. 21, at 3. The public awareness requirement, as codified in section 413.65(d)(4) and as quoted here, has been in effect since October 1, 2002. See 67 Fed. Reg. at 50,078, 50,089, 50,116.
- 6
These instructions mirror the ones that PM A-03-030 indicates should be used to reject a voluntary attestation submitted by the provider. See CMS Ex. 19, at 12-13.
- 7
Borgess alleged in its reconsideration request that the Borgess webpage screenshot attached to CMS's initial determination, titled "ProMed Physicians Family Practice" (and describing the ProMed clinics as "affiliates" of Borgess Health), omitted the "Borgess" wordmark that appeared at the top of the webpage. See CMS Ex. 32, at 4; compare id. at 63 (screenshot of ProMed Physicians Family Practice webpage showing the "Borgess" wordmark) and CMS Ex. 2, at 6 (screenshot of ProMed webpage without images or wordmark).
- 8
Borgess also alluded to consumer survey findings which, it said, demonstrated or confirmed that "patients are far more likely to have most recently received care from Borgess Medical Center than any other Borgess entity," that "public awareness of Borgess Health Alliance is negligible when compared to that of Borgess Medical Center," and that Michigan residents are more aware of Borgess Medical Center than any other Borgess entity. BMC Opening Br. to ALJ at 3 & n.3 (citing B. Ex. 10, ¶¶ 16-23 and B. Ex. 9, at 3-4).
- 9
CMS also objected to Borgess Exhibit 8, which Borgess later withdrew. ALJ Decision at 3.
- 10
In addition to a sign just outside its entrance door, the Mattawan clinic had a sign in, or near, its parking lot. That sign contained the name "Borgess," with the name "ProMed Family Practice" appearing below and in smaller type (CMS Ex. 3, at 2), in contrast with the clinic's entrance-door sign, which contained the name "ProMed Physicians" above the name "Borgess Health" (id. at 1). Borgess does not mention the parking-lot sign or dispute the ALJ's finding (ALJ Decision at 9) that differences between the entrance-door sign and the parking-lot sign had the potential to confuse patients or other members of the public about whether the clinic was part of Borgess Medical Center or merely part of the Borgess Health network.
- 11
Although we considered all of the arguments raised by Borgess in its request for review and reply brief, we have focused our analysis on the primary arguments, which, once addressed, render discussion of the secondary arguments unnecessary.
- 12
As Borgess asserts, CMS's version of this webpage omitted the banner containing the Borgess wordmark and photograph of the hospital campus (see CMS Ex. 13), but that omission is immaterial for the reasons stated in the text.
- 13
Another archived webpage (circa August 2010) submitted by Borgess listed two groups of "Family Medicine" offices – "Borgess Family Medicine Offices" (in Portage and Plainwell, Michigan); and "ProMed Physicians – Family Practice Offices" (in Portage, Richland, Three Rivers, and Mattawan, Michigan) – without indicating why one group operated (or appeared to operate) under the "Borgess" name while the other did not. B. Ex. 18, at 5.
- 14
As CMS accurately notes, the identification of the Richland and Three Rivers clinics as Borgess Health "affiliates" on Borgess's website during September 2014 does not differ from their identification on that website when Borgess first started treating them as provider-based. Compare CMS Ex. 7 (September 4, 2014 screenshot of Borgess.com webpage, identifying ProMed Physicians as an "affiliate" of Borgess Health) with CMS Ex. 11, at 1 (archived Borgess.com webpage dated November 2, 2007).
- 15
Borgess also discusses Mercy Hospital Lebanon, DAB CR3220 (2014), referencing it as the only other "substantive case[] discussing the public awareness standard." See B. RR at 6, 12-13. "It is well established that an ALJ decision is not precedent or binding on the Board." Medinn Corp., DAB No. 2928, at 11 (2019).
- 16
The "additional information" cited by the ALJ in John Hopkins was a patient brochure supplied by GSOC which stated that "[a]t [GSOC] . . ., you'll see the same faculty doctors and have access to the same high-quality outpatient cancer services available at the Johns Hopkins medical campus in East Baltimore," and which further advised patients that they would, if needed, "have access to the full range of services that has made Johns Hopkins a world leader in cancer care." DAB CR598, FFCL 2.d.
- 17
CMS provided an internet link to the OIG report (https://oig.hhs.gov/oei/reports/oei-04-12-00380.asp) in its response to Borgess's request for review.
- 18
The preamble to CMS's 2000 final rule states in relevant part:
Comment: A commenter questioned the requirement that services be furnished "under the name" of the main provider entity. The commenter argued that the requirement is inconsistent with the commenter's view that health care in the late 1990s is, and in many markets must be, "marketed" in a highly competitive environment. The commenter's view is that having provider-based status turn on the names used will inevitably invite micromanagement of the way the main provider's name is used by the department or other hospital-based entity.
Response: We [CMS] disagree with any suggestion that health care is merely a generic commodity that can be repackaged under another name for marketing purposes. On the contrary, we believe that operating under the name of the main provider, and holding oneself forward to patients under that name, is an important indicator of status as an integral and subordinate part of that provider. Therefore, we did not make any changes in the regulation based on this comment.
65 Fed. Reg. at 18,511.
- 19
For example, Borgess suggests that the ALJ's holding might preclude a provider-based facility that offers behavioral health, addiction treatment, or family planning services from omitting a hospital's name from an exterior sign in the interest of protecting patient privacy. B. RR at 17.
- 20
Adler, Jonathan H., Compelled Commercial Speech and the Consumer "Right to Know," 58 Ariz. Law Rev. 421 (2016).
- 21
We need not separately address whether the ALJ erred or abused discretion in admitting Borgess Exhibits 12, 13, and 14 over CMS's objections to those exhibits. ALJ Decision at 3. As we explain later, we vacate the ALJ's determination, in reliance on those exhibits, that, as of October 2, 2015, the Mattawan, Richland, and Three Rivers facilities met the public awareness requirement in 42 C.F.R. § 413.65(d)(4).
- 22
CMS understands Borgess's waiver argument as a claim that CMS is estopped from objecting to the ALJ's effective-date determination. See CMS Reply Br. at 9. Assuming Borgess intended to make an estoppel claim, we decline to entertain it because the Board is not authorized to decide an administrative appeal brought under 42 C.F.R. Part 498 based on equitable doctrines or defenses (such as equitable estoppel) and must decide them in accordance with applicable statutes and regulations, as we have done here. Kensington Diagnostics LLC, DAB No. 2992, at 16 (2019) (declining to rule on the merits of an equitable estoppel claim). Borgess has not in any event alleged, much less demonstrated, that the conditions for estoppel exist in this case. See id. (specifying the conditions for estopping the federal government).
