Monthly extreme heat forecasts will resume in April 2025.
Heat Affects Health in Many Ways
Warmer temperatures increase the risk for a diverse range of health risks. For example:
- An increased risk of hospitalization for heart disease.
- Heat exhaustion, which can lead to heat stroke if not treated, can cause critical illness, brain injury,
and even death. - Worsening asthma and chronic obstructive pulmonary disease (COPD) as heat increases the production of ground-level ozone.
- Dehydration, which can lead to kidney injury and blood pressure problems. Some kidney damage can become irreversible with repeated or untreated injury.
- Mental health and substance use risks, including loss of sleep and slowing of brain cognition, and heightened risk of increased acute psychiatric and substance use symptoms among people with chronic behavioral health conditions.
- Some medications increase the risk of heat-related illness. These include diuretic medicines (sometimes called “water pills”), antihistamine medicines (including many allergy medicines), and many antipsychotic medicines used to treat a variety of psychiatric and neurologic illnesses. Please review this list of common psychiatric medications that can impair the body’s normal ability to cool itself, as well as this list of tips for coping with hot weather for people who take medications.
Who is at high risk in the counties with the most extreme heat days?
People at elevated health risk from extreme heat exposure according to NIHHIS and CDC include those who:
- Have increased exposure (e.g., are experiencing homelessness, are emergency responders, are athletes, and/or work outdoors, or indoors with insufficient cooling);
- Have increased biologic sensitivity (e.g., are under age 5; are age 65 or over; are pregnant; and/or have chronic health conditions such as a mental health condition, diabetes, or cardiovascular condition); and/or
- Face high socioeconomic burden and/or additional barriers to accessing cooling or healthcare (e.g., are low income, live in a low resource community, and/or have one or more disabilities).
Check out your heat forecast for July along with top risk factors of concern in your county with our portal and learn how to protect people at elevated risk.
OCCHE Extreme Heat Tools and Resources
OCCHE and CDC have launched the Heat & Health Index (HHI), the first national tool to provide ZIP code-level heat-related illness and community characteristics data to measure vulnerability to heat. The HHI delivers a percentile ranking for each ZIP code so that public health officials, city planners, policymakers, and community members can identify areas that may be at increased risk of negative health outcomes from heat. It also details local factors that may be driving this risk, which can help inform interventions to protect public health and build a more heat-resilient future.
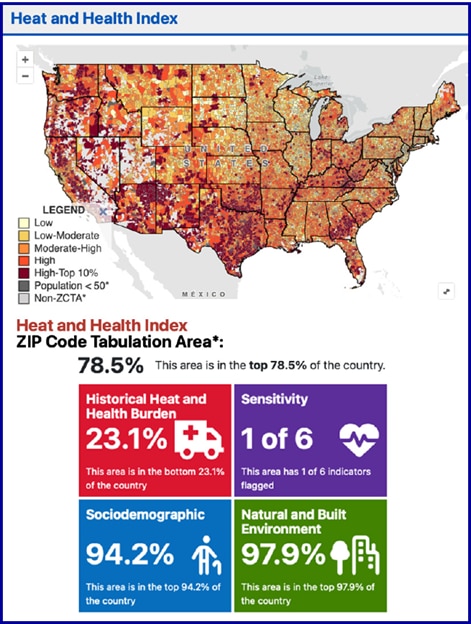
The HHI is comprised of four modules, made up of a total of 25 indicators. These modules are related to: vulnerability to heat (which provides information on historical temperatures and heat-related illness in a community); pre-existing health conditions that may increase sensitivity to negative health outcomes from heat; plus sociodemographic as well as natural and built environment characteristics that increase exposure or sensitivity to heat (or lessen one’s ability to cope with heat).
The HHI can be used to:
- Educate and inform the public about heat risk in their community;
- Identify and prioritize areas that may require special attention or additional action during the heat season to reduce heat-related illness; and
- Analyze the unique, local factors driving heat-related illness to help inform interventions to reduce heat risk over time.
Check out the Heat & Health Index to learn more about how different factors influence the way heat affects your community.
OCCHE and the National Highway Traffic Safety Administration (NHTSA) have launched a new resource called the Heat-Related EMS Activation Surveillance Dashboard, or the “EMS HeatTracker” for short. This first-of-its-kind tool maps EMS responses to heat-related illness across the country to help local decision makers and communities prioritize resources and interventions to prevent heat-related illness and save lives.
The EMS HeatTracker highlights jurisdictions (including all 50 U.S. States, Puerto Rico, and D.C.) and counties with the highest rates of heat-related EMS activations and allows for county- and jurisdiction-level comparisons to national averages in three categories in the prior rolling 30- and 14-day periods:
- population rate of heat-related EMS activations within a community;
- average EMS time in transit to reach a patient; and
- the percent of patients who are transported to a medical facility for further treatment.
The tool also provides national-level information on the number of heat-related EMS activations and the number of heat-related deaths among patients who were alive when EMS officials arrived on the scene. Demographic information is also available at the national level, including the age, race, gender, and urbanicity (i.e., urban, suburban, rural, and frontier) of patients.
The information displayed on the EMS HeatTracker is updated every Monday morning with a two-week lag behind real time.
Preparing At-Risk Populations for Extreme Heat
With increasing climate-related disasters like extreme heat, wildfires, and floods threatening health, resilience hubs are an emerging neighborhood-level strategy to prevent and mitigate the health impacts of climate change. Resilience hubs may have different names and functions in different places, but they are generally public-serving spaces (such as libraries, churches, or other trusted community spaces) that regularly provide resources such as health services, educational activities, and workforce development opportunities year-round, and provide shelter, food, water, medical aid, and access to communication and power during emergencies. By supporting community cohesion year-round, resilience hubs serve as a safe space that residents can trust and rely on during and after climate-related disasters.
La Familia Counseling Center (LAFCC) in South Sacramento has been providing multicultural counseling, outreach, and support services for children, youth, families, and individuals of diverse backgrounds for more than 50 years. LAFCC provided crucial testing and vaccination services to underserved populations throughout the COVID-19 pandemic. “We saw that our neighbors vulnerable to COVID-19 were also vulnerable to climate change,” says Rachel Rios, LAFCC’s Executive Director. “By bringing economic, educational, and clinical support to our neighborhood, we can help our neighborhood be resilient to the heat, floods, and wildfire smoke that threaten Sacramento.” LAFCC partnered with the Sacramento Promise Zone and leveraged a broad coalition of federal, state, and local partners to grow its resilience hub capabilities. LAFCC recently received grants from the California Department of Food and Agriculture’s Community Resilience Centers Program and from the U.S. Environmental Protection Agency’s Community Change Grants program to retrofit LAFCC’s Maple Neighborhood Center and to construct a new Opportunity Center. The Opportunity Center will provide employment training, mental health services, and community health resources, positioning LAFCC as a crucial support system for residents year-round and during crises. The Maple Neighborhood Center, already a trusted gathering space, will be upgraded with energy-efficient technology and renewable energy systems, increasing its capacity to serve the community during climate emergencies.

In summer 2020, air conditioning (AC) units were distributed in New York City (NYC) to low-income residents over age 60, and those with mobility impairments, to prevent heat-related illness. NYC officials developed the AC unit distribution program, a more expansive effort than traditional cooling assistance programs, in response to the co-occurring issues of extreme heat and COVID-19-related recommendations to stay home and avoid indoor public spaces, including cooling shelters. NYC government agencies, including Emergency Management, the Housing Authority, the Department of Health and Mental Hygiene, and the Department of Housing Preservation and Development Authority, worked together to distribute and install 16,000 AC units in public housing and 56,000 in private households. Participating agencies enrolled eligible residents who were already receiving benefits, community organizations that supported housing programs enrolled residents, and eligible residents were able to enroll themselves.
In a recent study partially funded by the National Institute of Environmental Health Sciences (NIEHS), researchers from Columbia and WE ACT for Environmental Justice evaluated the program's effectiveness in equitable distribution and health outcomes. They used NYC’s Heat Vulnerability Index to compare AC distribution to the Index’s map of residents most at-risk of adverse outcomes from heat exposure and found that AC distribution aligned closely to vulnerable areas and serving populations most in need. They also surveyed a sample of program participants and a comparable group of non-participants, which showed that installation of an AC unit had a positive effect on health during a summer when there were fewer public, cooled spaces available. Specifically, participants were less likely to report that hot weather made them feel sick in their homes compared to non-participants. As cities grapple with increasing extreme heat due to climate change, the NYC AC distribution program provides a model for supporting those most in need.
Extreme heat exposure can cause heat-related illnesses including heat stroke, heat exhaustion, cramps, fainting, and rashes. Outdoor workers, as well as indoor workers with insufficient ventilation or mechanical cooling, are at elevated risk for heat-related illness. One group of particular concern is agricultural workers, who often have physically demanding work outdoors through the hottest months and even during extreme heat waves. Recent studies have found that the average agricultural worker experiences 21 days (out of the average 153 day summer) of unsafe working days per year (i.e., days over 83.4°F) and the risk of heat-related death was more than 35 times higher for people working in agriculture compared to other occupations. The risks associated with unsafe working days are further compounded if nighttime temperatures are elevated or many excess heat days occur in a row.
There are an estimated 2.9 million agricultural workers in the U.S., of which a recent survey found that 78% self-identify as Hispanic and 70% as born outside of the U.S. Without protective measures, these workers are likely to experience even more heat-related illnesses as heat seasons become longer, hotter, and more intense. Important preventative measures for agricultural workers as well as all outdoor workers include providing water, shade, and breaks during the working day. The creation of culturally and linguistically appropriate training and resources related to heat protection and symptom identification can help migrant and seasonal agricultural workers protect themselves from the dangers of extreme heat. The OSHA field sanitation standard requires agricultural employers with 11 or more workers to provide drinking water. For more information on how to prevent, recognize, and treat heat-related illness, check out the Farmworker Justice and Migrant Clinicians Network Heat-Related Illness Clinicians guide. Migrant workers can also find helpful resources and more information about their employment-related rights in the U.S. at MigrantWorker.gov or TrabajadorMigrante.gov.

Image: Farmworkers exposed to sun and heat working in a strawberry field in Salinas, CA, wearing protective clothing including hats and long sleeve shirts. Source: iStock/rightdx.
Exposure to extreme heat can lead to increased stress, anxiety, and cognitive impairment. Research has shown that extreme heat is associated with several mental health outcomes including increased risk of suicide and increased mental health-related hospital admissions and emergency department (ED) visits. A recent study found that associations between heat and mental health-related ED visits were highest in the U.S. Northeast, Midwest, and Northwest regions. Furthermore, individuals with preexisting behavioral health conditions are at increased risk of heat-related illness or death from extreme heat. Psychotropic medications, which are commonly used in mental health treatment, as well as alcohol and other substances can contribute to this increased risk. A recent study on heat-related deaths found that 18% of deaths were due to alcohol poisoning (3%) and drug overdose (15%).
Resources:
- The CDC provides a list of common warning signs and symptoms of heat-related illness along with tips on what to do when you or someone you know is experiencing symptoms.
- Some medications increase the risk of heat-related illness. These include diuretic medicines (sometimes called “water pills”), antihistamine medicines (including many allergy medicines), and many antipsychotic medicines used to treat a variety of psychiatric and neurologic illnesses. Check out SAMHSA’s Tips for People Who Take Medication: Coping with Hot Weather for more information.

Figure: Heat map of all 50 U.S. states and District of Columbia. States with the largest increase in heat-related illness diagnoses over the assessment period are red, with less dramatic increases represented in shades of orange.
A recent publication from the U.S. Department of Veterans Affairs, Stanford University, University of Iowa, and CDC found that Veterans have been diagnosed with heat-related illnesses (HRIs), such as heat exhaustion and heat stroke, in all 50 states and that the rate of diagnosis has increased over time. The assessment utilized the Veterans Health Administration’s national electronic health record database to identify HRIs diagnosed from January 1, 2002, through December 31, 2019, and found that there were 33,114 documented cases of HRIs, which impacted 28,039 unique patients. The Veterans Health Administration is the largest integrated healthcare system in the United States, with 1,298 facilities serving over 9 million enrolled Veterans.
In addition to a statistically significant increase in the incidence of HRIs over time, the results raised important health equity concerns. Of note, Black and American Indian/Alaska Native Veterans were more likely to be diagnosed with HRIs. Veterans with existing medical conditions, including common comorbidities, also saw a greater increase in HRIs over time. For example, in 2022 ~50% of HRI diagnoses impacted Veterans with hypertension, but this increased to ~70% in 2019. The results demonstrated that there has been an increase in diagnosed HRIs among Veterans for nearly all U.S. states with a disproportionate increase of HRIs in California, Florida, and Texas. There were also notable increases in HRI diagnoses in other states such as Missouri, Arkansas, Virginia, Ohio, and New York. However, the rates for the Veteran homeless population were increasing in the first half of the assessment period, but then decreased in the second half of the assessment. This change in the trend occurred alongside the development and expansion of Veteran homeless programs, which suggests specific interventions can decrease the extent of heat related illnesses.
![Emergency Department Visits with a Diagnosis Directly Indicating Heat Exposure per 100,000 Population, 2016-2019. Source: Agency for Healthcare Research and Quality (AHRQ), Healthcare Cost and Utilization Project (HCUP), State Emergency Department Databases (SEDD) and State Inpatient Databases (SID), 2016-2019.]](/sites/default/files/nonsupp-heat-stcofips-2016-2019-alled.png)
In April 2022, Agency for Healthcare Research and Quality used the Healthcare Cost and Utilization Project (HCUP) 2016–2019 to estimate county-level population rates of emergency department (ED) visits with a diagnosis directly indicating heat exposure. The analysis was limited to records of ED visits, regardless of hospital admission, at community hospitals, excluding rehabilitation and long-term acute care facilities, with any-listed diagnosis directly indicating heat exposure. This analysis includes ED data from 2,550 counties in 39 States and the District of Columbia, representing 85 percent of the population and 81 percent of all counties in the United States in 2019. Among the 1,122 rural counties, 152 (13.5%) had heat-related ED visit population rates of 85 or more per 100,000 population (i.e., 90th percentile of population rates). In contrast, among the 344 large metropolitan counties, 8 (2.3%) had heat-related ED visit population rates in the 90th percentile. The report highlights that a larger proportion of rural than large metropolitan counties experience a high rate of heat-related illness, although there are more heat-related ED visits in large metropolitan areas (n=135,585 ED visits) than in rural areas (n=30,115 ED visits).
Pediatric vehicular heatstroke is one of the leading causes of non-crash, vehicle-related deaths for children 14 and younger. Since 1998, vehicular heatstroke has killed nearly 1,000 children. These deaths are preventable. Cars heat up fast, and when a child is left in a vehicle, that child's body temperature can rise to dangerous levels quickly.

These tips to prevent pediatric vehicular heatstroke could save a child’s life:
- NEVER leave a child alone in a vehicle, not even for a minute.
- Make it a habit to look in the back seat EVERY time you exit the car.
- Ask your childcare provider to call if your child doesn’t show up for care as expected.
- Place a personal item like a purse or briefcase in the back seat, as a reminder to look before you lock.
- ALWAYS lock the car and put the keys out of reach.
- If you see a child alone in a locked car, act immediately and call 911.
For communication resources to prevent hot car deaths, visit the National Highway Traffic Safety Administration’s (NHTSA) Vehicular Heatstroke Prevention page.
With lingering summer heat, it’s important to remember that high temperatures can have harmful effects on medications. Heat can degrade the active ingredients in medications, making them less effective when you need them most.
While asthma inhalers and epinephrine auto-injectors are often carried with you when you are away from home, they should not be stored in a hot car, even for short periods of time. Asthma inhalers contain aerosolized medicine that is sensitive to heat. "If left in a hot car, the pressure inside the inhaler can increase. In fact, inhalers can explode at high temperatures that can be reached in a closed car on a hot day. In addition, heat can reduce the potency of these inhaled asthma medications. Epinephrine auto-injectors must be stored at room temperature, between 68°F and 77°F, to maintain their potency. When exposed to temperatures above 86°F for prolonged periods, the epinephrine can degrade, compromising its efficacy in treating life-threatening allergic reactions.
Always store your medications in a cool, dry place, avoid leaving them in the car, and consider carrying them in insulated bags when traveling with them in warmer conditions. The U.S. Food & Drug Administration provides additional recommendations on the use of medicines affected by heat and other climate hazards.
Retrospective Heat Stories
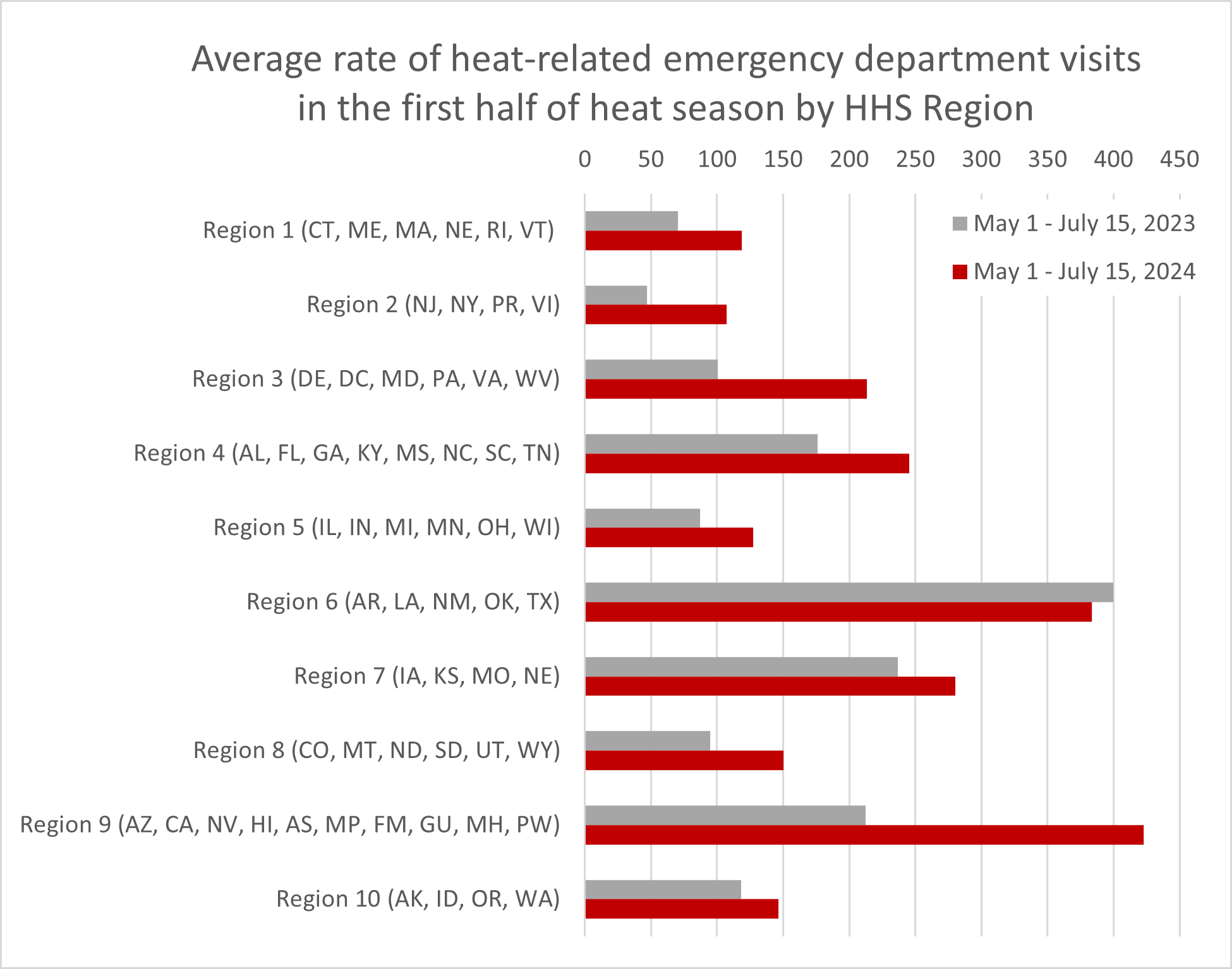
Figure. The CDC National Syndromic Surveillance Program (NSSP) provides daily rates of heat-related illness (HRI) by HHS Regions. NSSP is a network comprising CDC representatives, state and local health departments, and academic and private sector health partners jointly collecting and sharing electronic patient encounter data. NSSP includes ED visit data from approximately 80% of U.S. emergency departments covering 50 states, DC, and Guam.
The graphic above compares the average rate of HRI per 100,000 emergency department (ED) visits from May 1 to July 15 in 2023, with the average rate observed in 2024 for the same timeframe. The average HRI ED rates in 2024 are higher in 9 out of 10 HHS regions when compared to the average rates in 2023. Notably, HHS region 9 (which includes most of the Southwest and Hawai’i) is at nearly twice its already high 2023 rate, and the rates for HHS regions 2 and 3 (which include the mid-Atlantic region and Caribbean) are more than twice what they were this time last year.
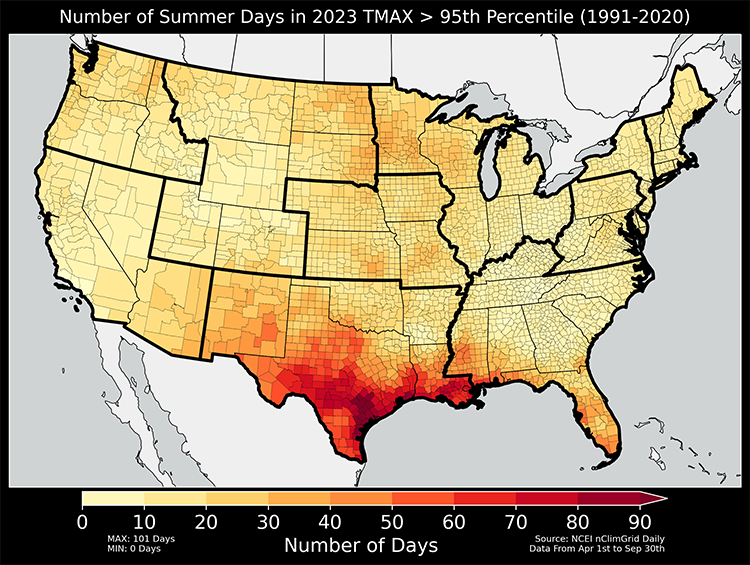
Figure: Temperature is calculated from NOAA’s nClimGrid-Daily v1-0-0, a 5km gridded dataset aggregated into counties for the contiguous U.S. For each day from April 1st to September 30th, a county’s temperature in 2023 is compared against its climatological normal from 1991–2020. Temperatures above the 95th percentile are considered abnormally hot for the region. Thick lines on the map indicate HHS regional boundaries:
Region 1: CT, ME, MA, NE, RI, VT
Region 2: NJ, NY, PR, VI
Region 3: DE, DC, MD, PA, VA, WV
Region 4: AL, FL, GA, KY, MS, NC, SC, TN
Region 5: IL, IN, MI, MN, OH, WI
Region 6: AR, LA, NM, OK, TX
Region 7: IA, KS, MO, NE
Region 8: CO, MT, ND, SD, UT, WY
Region 9: AZ, CA, HI, NV, AS, MP, FSM, GU, MH, PW
Region 10: AK, ID, OR, WA
2023 was the 5th-warmest year on record for the contiguous U.S. (average annual temperature 2.4°F above average). Texas, Louisiana, Mississippi, New Hampshire and Massachusetts each ranked warmest year on record while Maine, Vermont, Connecticut, Maryland, Virginia and Florida each ranked second warmest. The map above depicts the number of summer days in 2023 when a county’s maximum temperature exceeded its 95th percentile, thus indicating an abnormally hot day. Much of HHS Region 6, especially Texas and Louisiana, experienced more than 30 days of abnormally hot temperatures in 2023.

Figure: Table and plot of heat-associated deaths in Maricopa County in 2023 from the Department of Public Health’s latest report. Heat-caused deaths include cases where heat is listed as a direct cause of death on the death certificate, heat-related deaths include cases where heat is listed as contributing, and under investigation includes cases where the medical examiner suspects a heat-associated death.
Maricopa County, AZ is a highly populated county that experiences some of the U.S.’s most extreme heat. In 2023, there were over 100 days when the temperature was above 100° F. It also experiences high rates of heat-related illnesses. For example, it ranks in the 99th percentile of U.S. counties for their number of heat-related Emergency Medical Services (EMS) activations according to the National EMS Information System’s (NEMSIS) Heat-Related EMS Activation Surveillance Dashboard. In 2022, Maricopa suffered a record 425 confirmed heat-related deaths, after experiencing 339 confirmed in 2021. Through November 7, 2023, they had already confirmed 579 heat-associated deaths. Additional analysis gives insight into risk factors: 25% of the deaths occurred indoors, with air conditioning present but not functioning for 109 out of 146 of these cases. 45% of the deaths occurred among individuals experiencing homelessness.
This high number of heat-related deaths has prompted Maricopa County to take many actions including:
- Partnering with the Maricopa County Association of Governments, municipalities, universities, and community and faith-based organizations to form the Heat Relief Network to establish cooling centers and hydration stations;
- Providing surveillance via the county’s Department of Public Health to track heat-related illness and death in order to support heat relief planning and provide guidance for residents to protect themselves;
- Expanding access to heat relief by increasing evening and weekend hours and funding 2-1-1 Arizona to assist in finding transportation to the nearest Heat Relief location;
- Increasing funding to the HVAC repair and replacement fund; and
- Partnering with the state of Arizona to sign up for heat warning alerts.
According to the National Oceanic and Atmospheric Administration, May 2023 was the world’s third-warmest May on record and North America’s warmest May on record. Due in part to North America’s record- setting high temperatures, several hundred wildfires broke out across Canada in May, burning over 6 million acres and causing widespread air quality deterioration across much of Canada and the United States. Elsewhere in the world, Antarctic sea ice extent hit a record low in May and tropical cyclone Mocha made a devastating landfall as a Category 4 Cyclone in Myanmar on May 14. Earth’s ocean surface temperatures also set a record high for the second month in a row.
From August 31 through September 9, 2022, a record-breaking heat wave occurred across California. Temperature records were set in approximately 1,500 locales and excessive heat warnings were issued for much of the state. During this 10-day heat wave, an analysis by the California Department of Public Health (CDPH) found a 5% increase in deaths in the state – 395 more deaths than would be expected. The highest increases in deaths were seen among people aged 25-64, people who identify as Hispanic or Latino, and people from the South Coast region, including Los Angeles and neighboring counties. While we know from previous analyses that older adults and the very young are vulnerable to negative health impacts from extreme heat, CDPH notes that it is important for heat interventions to also consider the vulnerability of working-age adults, who may work in hot conditions or have other types of over-exposure to heat. CDPH believes the finding for the South Coast region may reflect where fewer residences have air conditioning, and where people are less acclimated to heat than inland residents.
This analysis highlights that we can likely expect heat impacts to extend into September in coming years. California has invested $404 million towards addressing extreme heat impacts, guided by the state’s Extreme Heat Action Plan. CDPH hopes that these findings will help guide future public health prevention, response, and resilience efforts as this plan is implemented.
During June–July 2021, the western U.S. experienced a record-breaking heat wave that lasted for several days. Estimated heat-related deaths and illnesses demonstrate the tragic toll of the heat wave on public health. Comparing the health records from June 26–July 10 between 2021 and 2020, heat-related deaths increased from 2 to 145 in Washington, 0 to 119 in Oregon, and 12 to 25 in California. These estimates were provided by the California Department of Public Health, Oregon Health Authority, and Washington State Department of Health. For context, the CDC estimates an average of 702 heat-related deaths per year for the entire U.S. (based on 2004–2018 data).
An article from the Administration for Strategic Preparedness and Response Technical Resources, Assistance Center, and Information Exchange features health care stakeholders sharing how lessons learned during the 2021 heat dome event and robust regional and local collaboration and communications during the pandemic facilitated connections during the heat wave in the summer of 2022.
Understanding the Hazard of Extreme Heat
The Wet Bulb Globe Temperature (WBGT) is a measure of heat stress on the human body, taking into account the effect of temperature, relative humidity, wind speed, and solar radiation on humans. Sweating can usually cool the body down to a stable internal temperature, but when the humidity is high, the air can become so saturated with moisture that the evaporation of sweat slows, hindering the body’s ability to cool itself.
Those who work or exercise in direct sunlight are particularly vulnerable to heat stress when the WBGT is high. Monitor the WBGT using the National Weather Service one-week WBGT forecast and take a break in an air conditioned building if you notice that you are sweating excessively while working or exercising outside.
Although early season extreme heat events are less common than those that occur later in the summer, they may be more deadly. As the summer progresses, our bodies get used to the higher temperatures and become more efficient at cooling, by increasing sweating rates, for example. When temperatures are very high early in the season, before our bodies have a chance to adjust, the risks of heat stress and heat stroke may be higher.
One study of heat waves in 43 U.S. cities found that the first heat wave in a community generally had greater impacts on mortality than heat waves that were not the first in the season. Heat-related mortality risk early in the heat season is even greater for those who are more vulnerable to the impacts of heat, such as young children, older adults, pregnant people, or those with chronic medical conditions that make them more susceptible to heat-related illness.
Because of the ways climate change increases temperature and temperature variability, these early season extreme heat events may become more common. Whenever temperatures are high, and particularly during extreme heat events in the early heat season, it is important to take precautions to protect yourself and those around you.
Resources for People at High Risk of Heat-Related Health Problems
Certain populations with limited resources may have restricted access to information on heat illness prevention, cool indoor environments, and government programs that provide critical support. Find more resources on heat illness prevention from Heat.gov and CDC websites.
Occupations that require strenuous work outdoors pose a high risk for heat-related illness. This includes construction workers, farmers, agricultural workers, delivery workers, athletes, landscapers, and others. Learn more about the dangers of working in heat. Employer responsibilities and resources for safety are also available through the Occupational Safety and Health Administration (OSHA) Heat Illness Prevention campaign.
- The Heat Safety Tool provides real-time heat index and hourly forecasts, specific to your location, as well as occupational safety and health recommendations from OSHA and the National Institute for Occupational Safety and Health (NIOSH).
- The National Institute of Environmental Health Sciences (NIEHS) Worker Training Program has heat safety and health training for at-risk workers.
- The Health Resource Services Administration (HRSA) funds National Training and Technical Assistance Partners — Farmworker Justice and Migrant Clinicians Network that helps clinicians prevent and treat heat-related illness among agricultural workers.
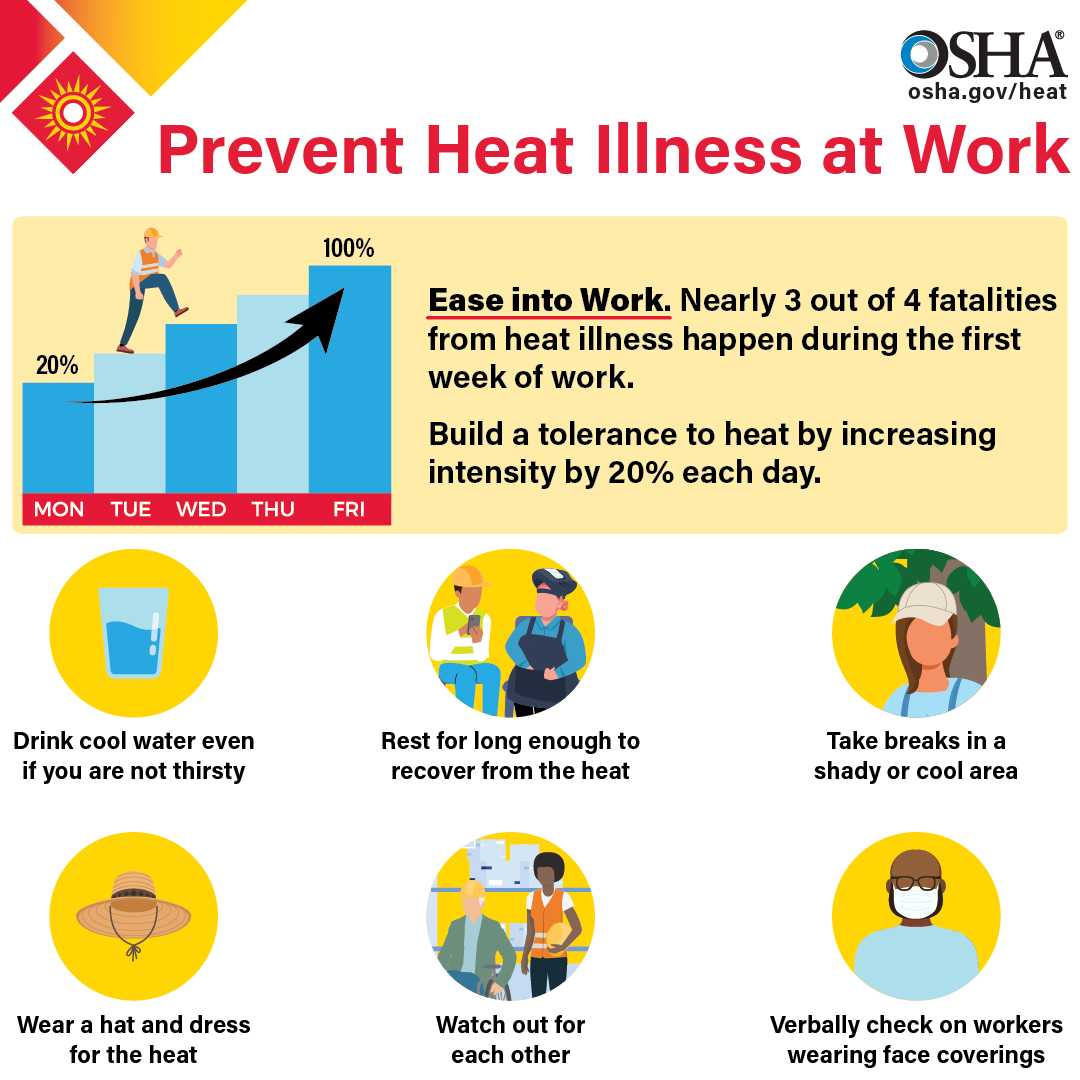
Image source: https://www.osha.gov/heat
A new resource from the National Integrated Heat Health Information System and the White House Extreme Heat Interagency Working Group highlights federal funding opportunities that are relevant to heat made available through the Inflation Reduction Act and the Bipartisan Infrastructure Law. These opportunities are open for applications from state, local, territorial, and Tribal governments; nonprofit organizations; manufacturers; and more. The webpage will be updated weekly as new funding opportunities become available.
- The Low Income Home Energy Assistance Program (LIHEAP) and the Weatherization Assistance Program (WAP) help keep families safe and healthy through initiatives that assist families with energy costs. To inquire about LIHEAP assistance, call the National Energy Assistance Referral (NEAR) hotline at
1-866-674-6327. - HHS has issued guidance that for the first time expands how LIHEAP can promote the delivery of efficient air conditioning equipment, community cooling centers, and more.
- The National Institute on Aging resource Hot Weather Safety for Older Adults offers background information on heat stroke, who is at risk, lowering your risk, and best practices.
- Medicare Advantage (MA) plans may provide Special Supplemental Benefits for the Chronically Ill (SSBCI) with equipment and services that improve indoor air temperatures and quality (such as portable air conditioners) to chronically ill patients.

Image sources: https://www.acf.hhs.gov/sites/default/files/documents/ocs/COMM_LIHEAP_Earth%20Day_FY2022.pdf, https://liheappm.acf.hhs.gov/datawarehouse
This CDC report on Heat Response Plans reviews steps emergency managers and health officials can take to develop and implement measures to protect their communities. Spikes in energy demand should be expected during summer months as air conditioning use increases. The combination of sagging power lines (copper expands as it heats up, thus increasing impedance and reducing throughput) and increased energy demands can cause power failures that make certain populations more vulnerable when the risk is highest. The HHS emPOWER program collects and shares de-identified Medicare data to help response agencies take action to protect the health of Medicare beneficiaries who depend on vulnerable electrical medical equipment.
Real-time information on health impacts from extreme heat can also help decision-makers implement strategies to reduce risk. CDC’s Heat and Health Tracker provides regular updates on the rate of heat-related Emergency Department visits (organized by HHS regions) and observed temperature.
If you are a local organization planning to open a cooling shelter, consider referring to CDC guidance on how to maintain a safe shelter during a heat wave.
Check out SAMHSA’s Tips for People Who Take Medication: Coping with Hot Weather for more information on how higher temperatures may impact your health if you are taking certain medications and steps to build resilience to climate impacts, as well as SAMHSA’s Climate Change and Health Equity site for more information on the behavioral health impacts of climate change, preparing for a disaster, and resources for disaster planning and climate change education.
A heat stroke is a medical emergency, and rapid recognition and aggressive early treatment are essential to reduce morbidity and mortality (as illustrated below).
See https://pubmed.ncbi.nlm.nih.gov/33856299/ for the full algorithm.
OCCHE’s Referral Guide summarizes resources that can address patients’ social determinants of health and mitigate health harms related to climate change. These resources include social services and assistance programs to which patients can be referred, as well as references for anticipatory guidance and counseling to help patients prepare for potential hazards.
Navigate to our other climate hazard pages below:
