Pesticide Exposure: Another Growing Hazard for Farmworkers in a Changing Climate
Climate change is altering many pest populations in the U.S., including via northern expansion of blacklegged tick populations, accelerated geographic spread and population growth of the spotted lanternfly, and increased duration of active periods of the codling moth, peach twig borer, and oriental fruit moth in California. This spread of agricultural pests, along with increased susceptibility of plants to invasive pests due to elevated CO2 and reductions in pesticide efficacy predicted with climate change, is increasing the use of pesticides—chemicals that are commonly used to manage pest populations.
Farmworkers, due to approximately 75% of pesticide use in the U.S. occurring in agricultural settings, and on the front lines of this increasing hazard. An estimated 10,000 to 20,000 pesticide poisonings among farmworkers are diagnosed in the U.S. annually. Workers applying pesticides face the highest exposure with their greatest exposure occurring during the mixing and loading processes (i.e., when the pesticides are in a concentrated state and there is a higher chance of spilling). Farmworkers working in sprayed fields are also at risk of high pesticide exposure and are less likely to use personal protective equipment (PPE) to protect themselves compared to those directly involved in the application process.
Acute health effects vary by pesticide type but can range from headache and dizziness to tremor and seizure. Acute occupational illnesses are tracked by the CDC-NIOSH Sentinel Event Notification System for Occupational Risk (SENSOR), a state-based surveillance program. In 2007–2011, 2,606 cases of acute occupational pesticide-related illness and injury were reported across 12 states. Of these cases, the rate of illness and injury among agricultural workers was 37 times greater than the rate for nonagricultural workers.
The hierarchy of controls provides a method of prioritizing safeguards to protect workers from hazards. Primary exposure control methods are hazard elimination or substitution by a less toxic substance. For pesticides, this could entail substituting insecticides most commonly identified in cases of injury and illness and utilizing integrated pest management practices on farms to reduce the need for chemical pesticides. Methods with lower effectiveness include providing and encouraging the use of PPE. PPE can be effective, but only when workers use it correctly and consistently, including when using during hot weather (a time when there may be concern about the heat burden of the PPE wearer).
Currently, there is an Agricultural Worker Protection Standard (WPS), which requires that employers of pesticide handlers and agricultural workers receive annual pesticide safety trainings. The Pesticide Education Resource Collaborative provides a library of EPA-certified educational resources to help the agricultural industry comply with the WPS. EPA is working on other ways to protect workers from pesticide risk.
Healthcare providers can help by learning to identify symptoms and treat patients with pesticide exposure from EPA’s Recognition and Management of Pesticide Poisonings manual. Unfortunately, pesticide poisoning symptoms can often be confused with symptoms of heat exhaustion, so also check out EPA’s comparison chart.
Increasing Vibrio Threat with Warming Waters
Vibrio are bacteria that naturally live in coastal waters. About a dozen Vibrio species can cause a human illness called vibriosis. Most people get vibriosis by eating raw or undercooked shellfish, particularly oysters. Some people get vibriosis after an open wound comes in contact with coastal waters or drippings from raw seafood.
Common symptoms of vibriosis include watery diarrhea, stomach cramps, nausea, vomiting, fever, and chills. One Vibrio species, Vibrio vulnificus, can cause severe and life-threatening wound infections. Many people with V. vulnificus infection need intensive care or limb amputation, and about 1 in 5 people with this infection die.
Around 1,400 culture-confirmed Vibrio illnesses are reported to CDC each year. Among these, 150–200 are V. vulnificus infections.
Warming Coastal Waters & Extreme Weather Events
Vibrio thrive in warmer waters, especially during summer months (May to October) and in moderately salty environments, such as estuaries. Warmer water temperatures along with more frequent and intense extreme weather events associated with climate change create favorable conditions for Vibrio bacteria to multiply and spread, which increases the risk for infection.
In the U.S., V. vulnificus infections have been most commonly reported by Gulf Coast states (Texas, Louisiana, Mississippi, Alabama, and Florida). However, the geographic range of V. vulnificus has been expanding northward along the Atlantic Seaboard by 48 kilometers per year, resulting in an eightfold increase in V. vulnificus infections in East Coast states from 1988 through 2018. These findings are likely explained in large part by climate conditions, such as water temperatures and salinity, becoming more favorable to Vibrio growth. During July and August 2023, the U.S. experienced above-average coastal sea surface temperatures and widespread heat waves. During the same period, several East Coast states reported severe and fatal V. vulnificus infections.
Extreme weather events also contribute to the spread of Vibrio. Coastal floods and hurricanes can force coastal waters into inland areas, putting people that are exposed to these waters at increased risk for Vibrio wound infections. This effect was observed in Florida after Hurricane Ian in 2022.
NOAA and partners have developed predictive models for Vibrio that can provide early warning signs of potential coastal hazards. Several experimental models predict the presence of V. parahaemolyticus and V. vulnificus in the Chesapeake Bay based on data from the Chesapeake Bay Operational Forecast System. Although these models cannot determine individuals’ risk for infection, they demonstrate the association between environmental conditions like water temperature, salinity, and chlorophyll and presence of Vibrio.
Anyone can get a Vibrio infection, but some medical conditions and treatments can increase a person’s risk for infection and severe complications. These include:
- Having liver disease, cancer, diabetes, HIV, or thalassemia
- Receiving immune-suppressing treatments
- Taking medicine to decrease stomach acid levels
- Having had recent stomach surgery
People who enjoy seafood and coastal activities—including swimming, fishing, or wading—can take steps to prevent a Vibrio infection.
- Do not eat raw or undercooked oysters or other seafood. Cook them before eating.
- Do not let raw seafood, its drippings, or its juices contaminate other foods.
- Always wash hands with soap and water after handling raw shellfish.
- If you are at increased risk for infection, wear protective gloves when handling raw seafood.
- If you have an open wound, stay out of coastal waters, if possible. This includes wading at the beach.
- Cover your wound with a waterproof bandage if it could come in contact with coastal waters or drippings from raw seafood.
- Immediately wash wounds and cuts thoroughly with soap and clean running water after contact with coastal waters or drippings from raw seafood.
- If you are at increased risk for infection, wear clothes and shoes that protect you from cuts and scrapes when around coastal waters.
Healthcare providers can prevent infections from becoming more severe by considering V. vulnificus as a possible cause of infected wounds that were exposed to coastal waters, particularly near the Gulf of Mexico or East Coast, and during periods with warmer coastal sea surface temperatures. Early antibiotic therapy and early surgical intervention improve survival. Clinical guidance is provided on CDC’s Vibrio website.
Tickborne Diseases and Conditions
Tickborne diseases—when a person has been bitten by a tick and gets sick—are increasingly threatening the health of people in the U.S. Tickborne diseases include Lyme disease, anaplasmosis, babesiosis, ehrlichiosis, spotted fever rickettsioses (including Rocky Mountain spotted fever), and tularemia, as shown on the map below. Lyme disease is the most common tickborne illness in the U.S., with an estimated 476,000 Americans diagnosed and treated for Lyme disease and an economic burden between $345 million and $968 million each year (in 2016 U.S. dollars). Early localized symptoms can include a rash at the site of tick bite (occurring in 70–80% of infected persons), fever, chills, malaise, fatigue, headache, muscle aches, joint stiffness, and swelling of lymph nodes. Patients who have Lyme disease are often not even aware of a tick bite before getting sick. Untreated Lyme disease can progress to disseminated disease and produce a wide range of symptoms including additional rashes, facial paralysis, an irregular heartbeat, and arthritis.

Figure: Geographic distribution of select tickborne diseases. For more information, visit the interactive map at https://www.cdc.gov/ticks/data-research/facts-stats/geographic-distribution-of-tickborne-disease-cases.html
Tick bites can also lead to conditions such as alpha-gal syndrome (AGS), a potentially life-threatening allergy to red meat and consumer products made from mammals. Evidence suggests that AGS is primarily associated with the bite of a lone star tick (Amblyomma americanum) in the U.S., but other kinds of ticks have not been ruled out. People with AGS have delayed allergic reactions to a sugar molecule called alpha-gal, which can be found in pork, beef, rabbit, lamb, venison, gelatin, and dairy. Patients with AGS have varying tolerance and sensitivity to products containing alpha-gal, and AGS reactions can vary, ranging from mild to life-threatening. A 2023 CDC report investigating testing data showed that there were more than 110,000 suspected cases of AGS between 2010 and 2022. Additionally, suspected cases are on the rise—from 2017 to 2021, there were approximately 15,000 new positive test results for AGS in the U.S. per year. Another CDC report identified gaps in healthcare provider awareness of AGS, finding 42% of participating healthcare providers had never heard of AGS. Therefore, the number of identified suspect cases of AGS from 2010–2021 is likely an underestimate of the true burden of disease because the diagnosis of AGS requires a clinical exam and a positive diagnostic test.
Climate change is one of several factors that affect when and where tickborne diseases and tick-associated conditions can occur.
- Increasing temperatures from climate change can influence tick life cycles by increasing a tick’s ability to reproduce. This can lead to larger tick populations and greater risk of germs spreading from tick bites to people.
- Additionally, milder winters and warmer early spring temperatures expand the seasons when ticks are active, resulting in more weeks of the year that people in the U.S. are at risk of tick bites.
- Changing climate patterns can also alter the natural environment and longstanding ecological relationships. The distribution and density of the wildlife ticks feed on (e.g., deer and small mammals) is changing, which can lead to an expanded geographic distribution (e.g., latitude, altitude) of the diseases and conditions associated with these ticks.
- Expanding tick ranges and increasing cases of disease are also linked to changes in land use patterns, such as reforestation, forest fragmentation, and suburban development, which can lead to increased opportunities for humans to be exposed to ticks.
Risk of tickborne disease varies based on time of year, time spent outdoors in tick habitat, and geographic region.
- Time of year: In areas of the eastern United States where Lyme disease is common, people are most likely to be bitten by blacklegged (deer) ticks during two times of the year: from April through July when nymphs are active, and again from September through November when adults are most active, though people can get bitten any time ticks are present.
- Time spent outdoors: Outdoor workers are at increased risk of tickborne diseases if they work at sites where ticks are common. Worksites with woods, bushes, high grass, or leaf litter are likely to have more ticks. Children ages 5 to 15 years are also at increased risk of tickborne diseases, especially if they play in tick-prone areas.
- Geographic region: Different climates throughout the U.S. support different species of ticks, which spread different diseases. Overall, the geographic range of infected ticks is expanding, putting an increasing number of communities at risk for tickborne diseases. Although the reported nationwide incidence of Lyme disease remained fairly stable from 2008 to 2019 at approximately 11 cases per 100,000 people per year, Vermont, Maine, Rhode Island, Pennsylvania, and West Virginia saw marked increases in Lyme disease incidence over the 10-year period. Data show that the majority of patients with AGS are adults living in the southern, mid-Atlantic, and midwestern regions.
How to Prevent Tickborne Diseases and Conditions
- Protect yourself from bites: Tick bite prevention is the first line of defense against tickborne diseases. Before you go outdoors apply EPA-registered insect repellents, treat clothing and gear with products containing 0.5% permethrin, and talk to your veterinarian about the best tick prevention products for your dog. Check out EPA’s webpage on Using Insect Repellents Safely and Effectively with extra guidance for applying repellents to children. If possible, when spending time outside, avoid wooded and brushy areas with high grass and leaf litter where ticks may live.
- Check for and remove ticks: After spending time outdoors, check your body for ticks, take a shower within 2 hours, and check your clothing, gear, and pets for ticks that may have caught a ride into your home. If you discover a tick on you or your pet, follow the recommended steps for proper tick removal as soon as possible. CDC’s Tick Bite Bot can assist you in removing attached ticks and seeking health care, if appropriate.
- Check your area’s risk: Check the current trends on tick exposure in your region at the Lyme Disease Data Dashboard and the Tick Bite Data Tracker, which shows Emergency Department visits for tick bites on a weekly and regional basis. CDC has additional interactive maps displaying tick surveillance data of four tick species and surveillance of tickborne pathogens identified in blacklegged and western blacklegged ticks.
Help your patients: The CDC’s Ticks website and Tickborne Diseases of the U.S.: A Reference Manual for Healthcare Providers have information on specific tickborne diseases including information on how to avoid tick bites, common symptoms, and treatment. CDC has also issued guidance on caring for patients after a tick bite.
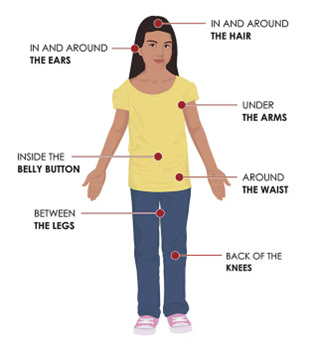
Figure. Places to check your body for ticks after being outdoors. Image from CDC.

Figure. How to remove a tick: (1) Use clean, fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible. (2) Pull upward with steady, even pressure. Don’t twist or jerk the tick. (3) After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water. (4) Dispose of a live tick by putting it in alcohol, placing it in a sealed bag/container, wrapping it tightly in tape, or flushing it down the toilet. (5) If you develop a rash or fever within several weeks of removing a tick, see your doctor. Image from CDC.
Mosquito-Borne Diseases
Mosquito-borne diseases—when a person has been bitten by a mosquito and gets sick—increasingly threaten the health of people in the U.S. Mosquito-borne diseases include West Nile virus (West Nile), dengue, malaria, Cache Valley, chikungunya, eastern equine encephalitis, Jamestown Canyon, La Crosse encephalitis, Rift Valley fever, St. Louis encephalitis, and Zika. Climate change is one of several factors that can influence when and where mosquito-borne diseases can occur. Climate factors could potentially affect mosquito-borne disease transmission through various mechanisms including:
- Increased temperatures and altered humidity, which is leading to:
- expanding geographic range of where mosquitoes live and transmit disease, including to higher latitudes and elevations;
- accelerating the rate that mosquitoes bite;
- accelerating mosquito development and reproduction rates, potentially leading to higher mosquito populations; and
- accelerating virus replication and parasite development within mosquitoes, allowing them to become infectious more quickly and transmit diseases faster.
- Altered precipitation patterns and more extreme storms. Both flooding (creating standing water) and drought (leading to water storage practices) can increase the number of sites where mosquitoes lay eggs. Mosquitoes generally do not survive the high winds and flooding that hurricanes bring, but mosquito eggs can survive. Therefore, it is common for mosquito populations to decrease during and immediately after a hurricane, and then grow rapidly. Water accumulation is critical for immature mosquito development, and humidity is important for adult survival.
- Milder winters, earlier springs, and longer and warmer summers, expanding the season for mosquito-borne disease transmission.
These climate impacts could also interact with human activities, such as spending more time outdoors, urbanization, deforestation, and increased global travel, to further amplify disease transmission risks.
WNV, primarily spread to people through bites of infected Culex mosquitoes, is the most common mosquito-borne disease in the continental U.S. Many U.S. counties now report West Nile cases, but the Great Plains and western states are more likely to have high incidence. Approximately 80% of people infected with WNV will not have any symptoms, 20% will experience flu-like symptoms, and less than 1% will develop severe West Nile neuroinvasive disease (WNND), a condition that can lead to death or long-term disability. Older adults and those with compromised immune systems are at higher risk for WNND. Currently, no medicines or vaccines are available for West Nile.
- This year marks the 25th anniversary of the first detection of WNV in people in the U.S. WNV has caused 59,000 infections and 2,900 deaths between 1999 and 2023 (and likely more because many people don’t have symptoms).
- West Nile prevention depends on community-level mosquito control programs to reduce mosquito vector densities, personal protective measures to decrease exposure to infected mosquitoes, and screening of blood and organ donors. Despite progress in the fight against WNV, current prevention methods are not enough to reduce the burden. It is normal for West Nile cases to vary in number and location by year in the U.S., making it difficult to predict or identify any one reason for a higher-than-average year. Public health needs more ways to detect outbreaks early, control mosquitoes, and treat and prevent the disease to effectively protect people from WNV.
Dengue virus, spread to people through bites of infected Aedes species mosquitoes (Ae. aegypti or Ae. albopictus), is common in six U.S. territories and freely associated states, and outbreaks have recently occurred in Florida, Hawai’i, Texas, Arizona, and California. About 25% of people infected develop symptoms, including fever with aches and pains, nausea and vomiting, or rash. Less than 5% of dengue infections progress to severe disease, which can lead to hospitalization and death. Early diagnosis and supportive medical care are essential in severe cases, though no specific treatments are available. A vaccine is being implemented in Puerto Rico for children 9–16 years old who have laboratory-confirmed evidence of previous dengue infection.
- In 2024, there have been over 10 million dengue cases across the Americas, significantly surpassing the 4.6 million cases reported for the entirety of 2023—already a record year for dengue. After a decade of almost no dengue transmission, Puerto Rico is now facing an outbreak ahead of the typical dengue season (starting in August). The Puerto Rico population has limited immunity to the strains of dengue currently circulating, and repeat infections raise the risk for hospitalization and severe disease. The observed limited immunity, combined with a prolonged period of low transmission, could lead to an outbreak with greater magnitude and severity.
- As of July 2024, more than 50% of dengue cases in Puerto Rico have required hospitalization, with over 1,100 hospitalizations reported. The U.S. Virgin Islands have also reported dengue cases, and travel-associated cases in the continental U.S. are higher than previous years, increasing the risk of local transmission in areas wit Aedes mosquitoes and conducive climatic conditions.
For the first time since 2003, the U.S. has had locally acquired cases of malaria in Florida, Texas, and Maryland. Malaria is a serious mosquito-borne disease caused by different species of Plasmodium parasites that infect Anopheles species mosquitoes. People typically become infected with malaria following the bite of a mosquito carrying the parasite.
There are about 2,000 reported cases of malaria in the U.S. each year, mostly in travelers returning from other countries. Continuous spread of malaria was eliminated in the U.S. in the early 1950s through mosquito surveillance and control measures; however, as we’ve seen this summer, locally acquired malaria cases do still occur in the U.S.
Anopheles species mosquitoes can be found in much of the continental U.S., making local spread possible if people infected in a malaria-endemic country travel to the U.S. and are bitten by local Anopheles mosquitoes, which can then become infected and spread the parasite to people who have not traveled. The risk for local transmission is higher in areas where local climatic conditions allow Anopheles mosquitoes to survive during all or most of the year. Temperatures also need to be warm enough for the malaria parasite to develop in the mosquito. This summer, the U.S. has had plenty of the hot and humid conditions in which mosquitoes thrive, as well as increased international travel, potentially contributing to local spread.
While local malaria transmission in the U.S. is rare, it is possible that increased temperatures and altered precipitation patterns and humidity due to climate change may lead to increased mosquito populations, increased range of Anopheles mosquitoes, a greater number of mosquito biting days, and faster development of the malaria parasite in mosquitoes, all of which could impact local transmission in the U.S. in the future.
Prevention of Mosquito-Borne Diseases
The best way to prevent any mosquito-borne disease is to protect yourself from mosquito bites. When outside, use an Environmental Protection Agency-registered insect repellent (follow these tips for applying insect repellent on children from the American Academy of Pediatrics) and wear loose-fitting, long-sleeved shirts and pants. Control mosquitoes in and around your home by installing screens on windows and doors and using air conditioning when available plus eliminating standing water (such as in outdoor buckets, planters, or bird baths) where mosquitoes breed. Children aged 9-16 years old who live in dengue-endemic areas and have laboratory confirmation of a previous dengue infection should get a dengue vaccine. For additional information, check out CDC’s Fight the Bite site with information on preventing bites from both ticks and mosquitoes, additional recommendations for if you are traveling to a place where a mosquito-borne disease is endemic, and recommendations for workers.
Climate change is one of several factors that can influence the distribution and prevalence of vector-borne diseases. Among vector-borne diseases in 2023, Lyme disease (tickborne) as well as West Nile virus, dengue, and malaria (mosquito-borne) were of public health concern in the United States. Lyme disease is the most common vector-borne illness in the United States, with an estimated 476,000 people diagnosed and treated each year. Traditional Lyme disease surveillance data are available through 2021 from CDC. In 2023, 2,406 West Nile virus disease cases were identified across 47 jurisdictions, including 1,599 neuroinvasive disease cases. There were also 2,556 dengue cases across 52 jurisdictions, including locally acquired dengue cases in Florida (n=168), California (n=2), Texas (n=1), and Puerto Rico (n=933; where dengue is endemic). The vast majority of malaria cases in the United States are travel-related, usually by people who travel to countries where malaria is endemic (regularly occurring). During May–October of 2023, though, the United States had a total of 10 cases of locally acquired malaria reported in Florida, Texas, Maryland, and Arkansas (as of October 19, 2023).

Figure: Number of West Nile virus human disease cases in the United States over the past decade. Data from CDC (2023 data are preliminary and subject to change).
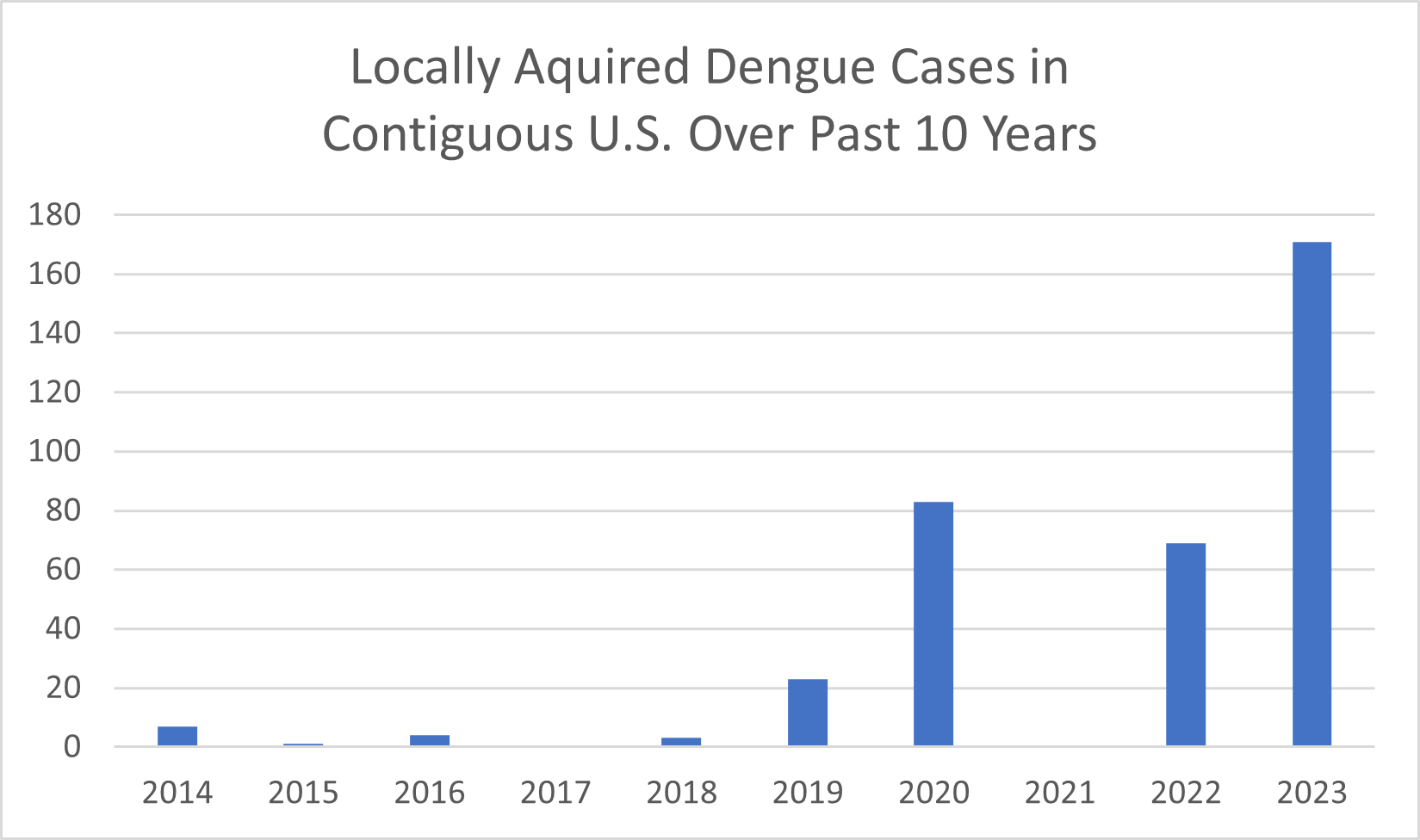
Figure: Number of locally acquired dengue cases in the contiguous U.S. over the past decade. Locally acquired cases occurred among people with no history of travel to a dengue-endemic region in the two weeks before illness onset. Data from CDC (2023 data are preliminary and subject to change).
Navigate to our other climate hazard pages below:
