A guide for health care providers to start the vaccine conversation with patients and to provide answers to common questions about flu, COVID-19, and RSV.
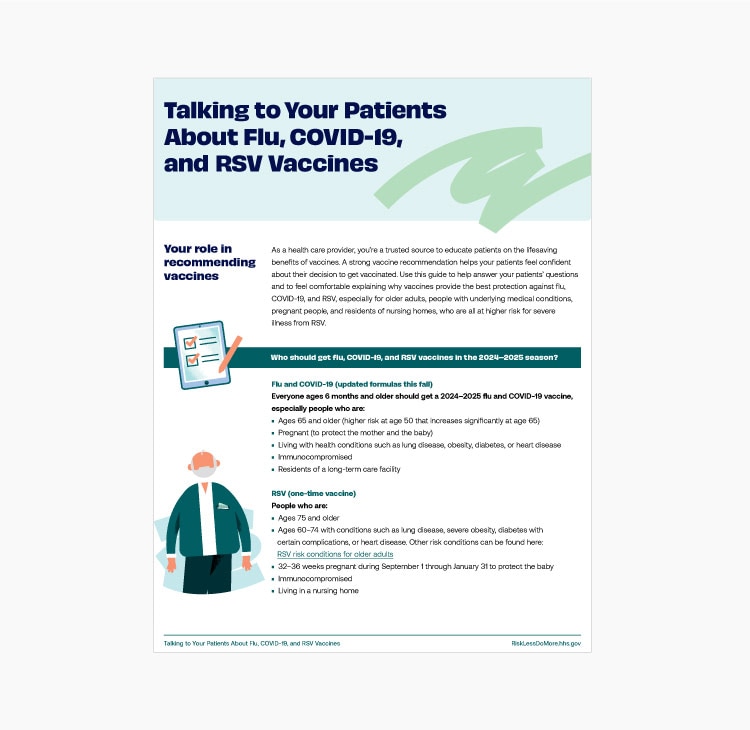
Your role in recommending vaccines
As a health care provider, you’re a trusted source to educate patients on the lifesaving benefits of vaccines. A strong vaccine recommendation helps your patients feel confident about their decision to get vaccinated. Use this guide to help answer your patients’ questions and to feel comfortable explaining why vaccines provide the best protection against flu, COVID-19, and RSV, especially for older adults, people with underlying medical conditions, pregnant women, and residents of nursing homes, who are all at higher risk for severe illness from RSV.
| Flu and COVID-19 (updated formulas this fall) | RSV (one-time vaccine) |
|---|---|
Everyone ages 6 months and older should get a 2024-2025 flu and COVID-19 vaccine, especially people who are:
| People who are:
|
Starting the vaccine conversation
All patients:
- Use clear, specific language: “It looks like you’re due for your flu and COVID-19 vaccines, and you haven’t had an RSV vaccine before. Because you’re over 75, you’re more likely to get very sick or need hospital care if you get one of these illnesses. Vaccines cut your chances of being hospitalized by half or more.”
- Share your personal experience: “Flu, COVID-19, and RSV spread fast this time of year. Every year, our office sees a lot of patients who are very sick from one of these infections. For people who are recommended to get them, these vaccines cut the risk of getting really sick or being hospitalized by half or more.”
- Emphasize the benefits: “I recommend flu, COVID-19, and RSV vaccines for you because they cut your risk of getting really sick or being hospitalized by half or more.”
- Ask follow-up questions: “Do you have any questions or concerns I can help answer about vaccines?”
Patients who express vaccine hesitancy:
- Acknowledge concerns and opposition: “I understand that you’re worried about vaccine side effects and that’s perfectly normal. Is there any more information I can give you to help ease your concerns?”
- Don’t hesitate to try again: “I respect your decision. Let’s revisit the topic at your next appointment. In the meantime, I’m happy to answer any questions you may think of.”
- Give advice from your personal experience: “I understand your concern, but I will tell you – not only did I get vaccinated, but I made sure my parents/kids/family have been vaccinated, too.”
| If your patient says... | You can say... |
|---|---|
| Can I get more than one vaccine at the same time? |
|
| Flu vaccines cause flu. |
|
| I got a flu vaccine last year. Why do I need another one? |
|
| COVID-19 vaccines cause long-term side effects. |
|
| I already got a COVID-19 vaccine. Do I really need another one? |
|
| RSV vaccines are too new and haven’t been studied enough. |
|
Starting the vaccine conversation with pregnant patients
All patients:
- Use clear, specific language: “It’s RSV season, and infants have a high risk of getting severely ill from RSV. If you’re 32 through 36 weeks pregnant between September 1 and January 31, one option* to protect your baby against RSV is to get the maternal RSV vaccine.”
- Share your personal experience: “Many of my pregnant patients get vaccinated to protect their babies from the moment they’re born through their first 6 months, when your baby is at risk from flu, COVID-19, and RSV.”
- Emphasize the benefits: “RSV causes more infant hospital stays than any other illness. Getting vaccinated yourself cuts your baby’s risk of being hospitalized with RSV in their first 6 months of life by more than 70%. Flu and COVID-19 vaccines also provide protection for you and for your pregnancy.”
- Ask follow-up questions: “Do you have any questions or concerns I can help answer about vaccines?”
*Patients who cannot or opt not to get a maternal RSV vaccine can still protect their babies by having them immunized soon after birth with nirsevimab, an antibody that provides protection during an infant’s first 6 months.
Patients who express vaccine hesitancy:
- Acknowledge concerns and opposition: “I understand that you’re worried about getting vaccinated during pregnancy and that’s perfectly normal. Is there any more information I can give you to help ease your concerns?”
- Don’t hesitate to try again: “I respect your decision. Let’s revisit the topic at your next appointment. In the meantime, I’m happy to answer any questions you may think of.”
- Inform your vaccine-hesitant patients about another RSV preventive: “If you decide not to get an RSV vaccine during pregnancy, your newborn can still get protection from severe RSV through an immunization soon after birth that gives the baby antibodies needed to fight RSV infection.”
| If your patient says... | You can say... |
|---|---|
| Is it safe for me to get vaccinated during pregnancy? Is it safe for my baby? |
|
| Can I wait until after my baby is born to get vaccinated? |
|
| Why do I need an RSV vaccine if I’m not at high risk for RSV? |
|
